Health insurance is meant to protect patients—not trap them in endless paperwork, surprise bills, and unclear explanations. Yet each year, millions of claims are rejected for reasons ranging from minor data errors to systemic payer policies. Understanding health insurance claims denial rates and broader health insurance claim denial statistics is no longer optional—it’s essential for patients, employers, providers, and policymakers who want clarity in an increasingly complex system.
The team at HealthsureHub analyzed the latest datasets, compared payer performance, and broke down what truly drives denial rates so consumers can make informed decisions backed by real numbers—not insurer marketing. This deep dive helps uncover why insurance companies deny claims and highlights the top insurers by denial rate.
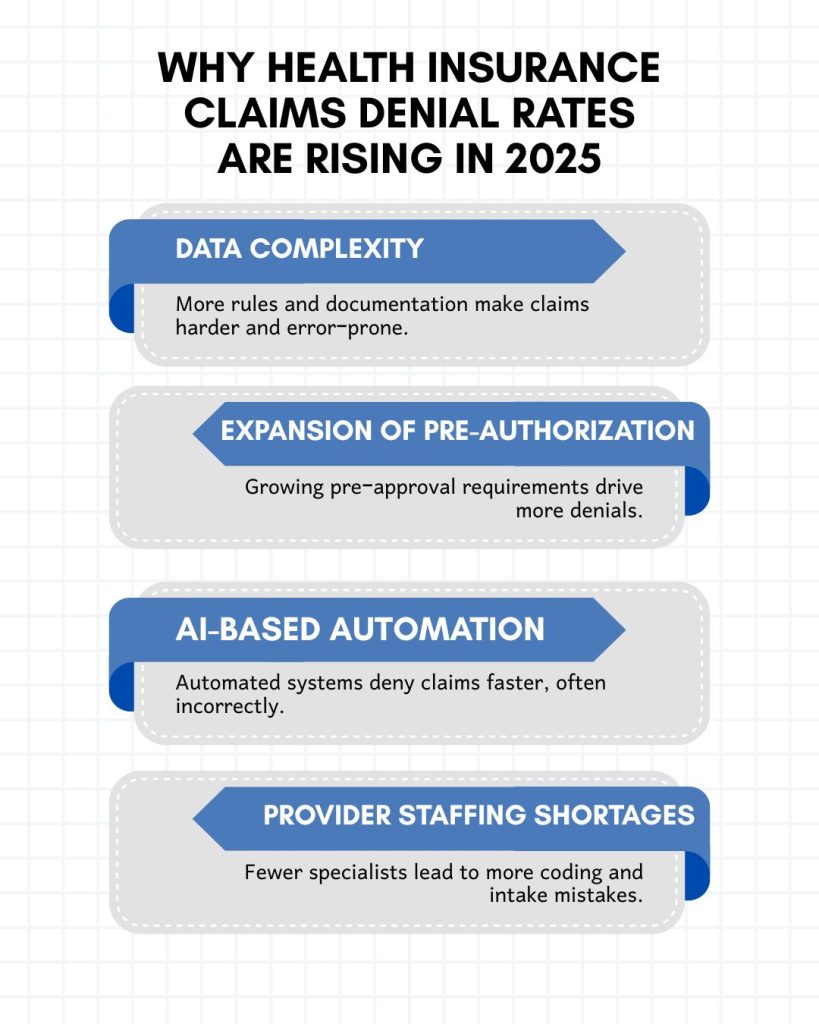
Why Health Insurance Claims Denial Rates Are Rising in 2025
Across federal marketplace data, provider surveys, and payer transparency reporting, one trend is clear: denial rates are climbing, and they have been for several years. A combination of factors drives this rise:
- Data complexity– more coding rules, more documentation requirements, more payer policies. Even experienced billing teams struggle to keep up, contributing to systematic insurance claim processing issues.
- Expansion of prior authorization- insurers increasingly require pre-approval for common services, and failing to secure it is now one of the fastest-growing denial reasons.
- AI-based automation- many payers now use automated tools to review and deny claims at high volume. While efficient for insurers, these systems often misclassify claims, reject medically necessary care or deny claims instantly without human overview.
- Provider staffing shortages- health systems face fewer revenue cycle specialists, leading to more intake errors and coding mistakes, worsening revenue cycle management challenges.
When all of these pressures collide, health insurance claims denial rates rise sharply, and it’s the consumers who pay the price.
What is the current denial rate for healthcare claims?
Healthcare claim denials continue to climb, creating ongoing financial strain for providers. More than half of healthcare organizations—54%—report that denial rates have increased in recent years, making it harder to predict when, or even if, they will receive payment for the care they’ve delivered.
Wasted spending tied to claims processing has also ballooned. In 2009, inefficiencies in the system cost the U.S. healthcare sector an estimated $210 billion. By 2019, that figure had grown to $265 billion, reflecting a decade of rising administrative burden and mounting denial challenges.
Adding to this pressure, 41% of providers say that at least one out of every ten claims they submit ends up denied, forcing teams to redo work, chase missing documentation, and absorb revenue losses they can’t afford.
Despite advances in technology, many claims are still tripped up by preventable errors, delays, or data mismatches—problems that continue to drive denial rates upward. Today, according to the latest Experian Health survey, it states that:
- At least 10% of claims are denied for many providers
- Nearly seven in ten (68%) report that denials often stem from incorrect or incomplete patient information collected during intake.
- Just 56% feel confident that their existing claims technology is capable of supporting today’s revenue cycle challenges.
- And in response, 59% say they expect to invest in tools specifically designed to reduce denials within the next six months.
These numbers emphasize the urgent need to understand the common reasons for denied health insurance claims and implement strategies for how to reduce insurance claim denials.
Which Insurance Companies Have the Highest Denial Rates?
Federal ACA marketplace transparency data is the most reliable source available because insurers are legally required to report their denial statistics.
Some insurers consistently reject far more claims than others, creating serious obstacles for patients who expect their policies to protect them when they need care the most. Oscar Health wins the race around 26% denied rates of all in-network claims followed by:
- Molina Healthcare with denied rates around 22%
- Ambetter with denial rates falling around 14%
- United Healthcare with 19% denied rates
Through its detailed analysis, HealthCareHub identified a significant shift at UnitedHealthcare: since 2023, the company’s claim denial rate has dropped sharply, reaching 19% in 2024. These insurers consistently deny more than 1 out of every 4 claims—numbers that profoundly affect patients who rely on them for essential care.
What Are the Biggest Drivers of High Denial Rates?
1. Missing or inaccurate patient data
A significant portion of claim denials—more than 25%—can be traced back to simple data errors during patient intake. Even small mistakes, such as a misspelled name, outdated insurance information, or an incorrect date of birth, can cause a claim to be rejected outright. As administrative workloads increase, these data-entry issues become more common, adding unnecessary delays and contributing heavily to rising health insurance claims denial rates.
2. Prior authorization requirements
Prior authorization remains one of the most frustrating obstacles for both patients and providers. Many insurers require pre-approval for treatments, medications, imaging tests, and even standard procedures. If authorization isn’t obtained in time—or if rules change without notice—claims can be delayed or denied. This creates a bottleneck that slows down care and often results in patients being stuck in a cycle of back-and-forth paperwork rather than receiving the treatment they need.
3. Medical necessity disputes
One of the most contentious denial reasons is when insurers classify a doctor-recommended service as “not medically necessary.” These disputes place insurers in direct opposition to clinical judgment, forcing physicians to justify treatments they deemed essential. This not only frustrates providers but also leaves patients vulnerable to unexpected medical bills. Medical necessity denials have been increasing, making them a major contributor to high health insurance claims denial rates nationwide.

Source: Pexels
4. Coding or billing mistakes
With thousands of medical codes, frequent regulatory updates, and payer-specific requirements, even the most experienced billing teams can make errors. A single incorrect CPT, ICD-10, or modifier code can cause a claim to be rejected. These mistakes often require extensive rework, slowing down reimbursements and increasing administrative costs. As coding becomes more complex, these errors contribute significantly to the industry-wide rise in denials.
5. Policy lapses
Even a short lapse in coverage can lead to an automatic denial. When premiums are missed—sometimes by only a few days—patients may unknowingly receive care while uninsured. Providers submit the claim, only to discover that the policy was inactive at the time of service. This leaves both patients and healthcare organizations facing unexpected financial burdens, further complicating the claims landscape.
Together, these factors form a perfect storm that drives up health insurance claims denial rates. What ties all of them together is the increasing complexity of U.S. healthcare administration—from eligibility checks to coding rules to evolving payer policies. As the system becomes harder to navigate, denials naturally follow, leaving providers overwhelmed and patients caught in the middle.
Conclusion
As the healthcare system grows more complex, understanding health insurance claims denial rates has become essential—not just for industry professionals, but for patients, employers, and policymakers who depend on timely, accurate coverage.
The data makes one thing clear: denial rates are not slowing down, and consumers can no longer assume their claims will be approved without challenges. By tracking insurer performance, improving data accuracy, and demanding greater transparency from payers, both patients and providers can better protect themselves from unexpected costs and ensure that medically necessary care is properly covered. Ultimately, staying informed about health insurance claims denial rates is the strongest defense against a system where reimbursement is far from guaranteed.
Sources:
https://www.experian.com/blogs/healthcare/healthcare-claim-denials-statistics-state-of-claims-report
https://www.cnbc.com/2019/10/07/study-reveals-265-billion-wasted-on-health-care-each-year-in-us.html
https://www.nber.org/research/data/affordable-care-act-aca-exchange-data
https://www.billing-coding.com/full-article.cfm?articleID=6976
https://www.ncbi.nlm.nih.gov/books/NBK53908
https://www.valuepenguin.com/health-insurance-claim-denials-and-appeals
https://www.moneygeek.com/insurance/health/aca-claim-denial-rates-by-state-and-insurer