Neck pain is one of the most frequently reported musculoskeletal complaints in clinical settings, making accurate ICD-10 coding essential for clean claims, proper documentation, and consistent symptom tracking.
Understanding the ICD-10 code for neck pain is especially important for providers, coders, and billing teams who want to avoid denials and ensure diagnosis codes match the patient encounter. In this article, our team at Healthsure Hub reviews the ICD-10 code for neck pain, explains how it is used, and outlines documentation tips to support accurate coding.
What Is the ICD-10 Code for Neck Pain?
The ICD-10 code for neck pain is M54.2, which is used to report general cervical pain without specifying an underlying cause. This code applies when the provider documents neck pain as a symptom but does not identify a more specific diagnosis such as radiculopathy, trauma, or a structural condition. It is appropriate for a wide range of clinical encounters including primary care, chiropractic, physical therapy, orthopedics, and urgent care visits.
Neck pain is also a widespread global issue, affecting 203 million people worldwide in 2020, with prevalence remaining stable over recent decades and projected to increase significantly by 2050 due to population growth and aging. Because M54.2 classifies neck pain broadly, it is commonly used when symptoms are non-specific, newly onset, or part of a routine evaluation.
When Should ICD-10 Code M54.2 Be Used?
The ICD-10 code for neck pain, M54.2, should be used when the patient’s main documented symptom is non-specific neck pain, and no more precise diagnosis is identified during the visit. It applies when discomfort is present but not linked to a confirmed injury, neurological condition, or structural issue. M54.2 is appropriate in situations such as:
Generalized cervical pain or stiffness
When a patient reports broad neck discomfort without clear localization or cause, M54.2 accurately reflects this non-specific presentation.
Non-specific neck tightness
If the provider documents tightness or tension in the cervical area but does not diagnose a muscle spasm or another defined condition, M54.2 is appropriate.
Strain-like symptoms without a confirmed injury
Patients sometimes describe their symptoms as “feeling like a strain,” but unless an actual strain or injury is diagnosed, M54.2 should be used rather than trauma-related codes.
New or undifferentiated neck discomfort
For patients experiencing early, unclear, or mild symptoms, M54.2 can be used until further evaluation clarifies whether a more specific diagnosis exists.
Neck pain related to posture or repetitive strain (when not otherwise specified)
If documentation indicates pain from prolonged sitting, poor posture, or repetitive motions but does not confirm a specific pathological condition, M54.2 is an appropriate general diagnosis.
If the provider identifies a more specific cause, such as radiculopathy, disc disorder, or whiplash, a different ICD-10 code should be selected. Proper code choice always depends on what is documented in the patient record.
Documentation Requirements for M54.2
To support ICD-10 Code M54.2, documentation should include:
- The patient’s description of neck pain
- Onset, duration, and severity
- Aggravating or relieving factors
- Functional impact (e.g., limited range of motion)
- Relevant history
- Whether neurological symptoms are present
- Physical exam findings
Clear documentation ensures the diagnosis is justified and helps prevent medical record ambiguity during audits or payer reviews.
Common Coding Mistakes With M54.2
Even though the ICD-10 code for neck pain is a straightforward code, several common billing errors can still lead to claim issues:
- Using M54.2 when a more specific diagnosis is documented: If documentation identifies radiculopathy, trauma, or cervical disc disorder, a different code may be required.
- Pairing M54.2 with conflicting codes: Coding both “non-specific neck pain” and a confirmed pathology may cause inconsistent documentation.
- Missing documentation of symptoms: Payers may deny claims when neck pain is listed without supporting details in the record.
- Using M54.2 for chronic pain without clarity: If the provider states “chronic neck pain,” coders may need a chronic pain code in addition to, or instead of, M54.2, depending on documentation.
By understanding these common pitfalls and ensuring documentation matches the patient’s presentation, providers and billing teams can reduce denials and maintain more accurate coding when using M54.2.
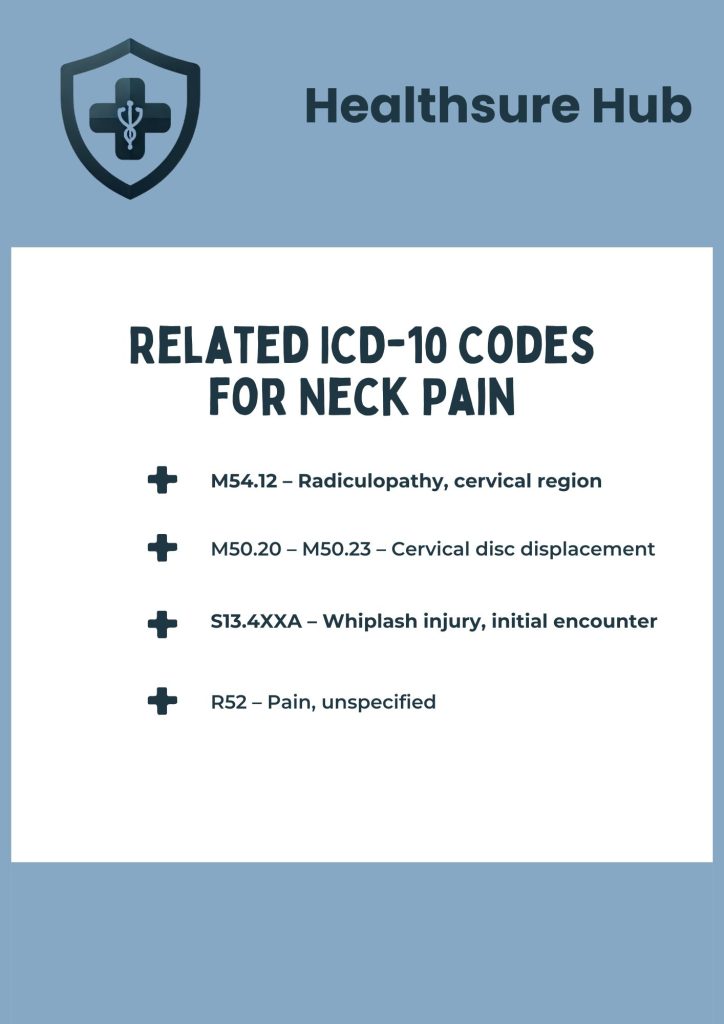
Related ICD-10 Codes for Neck Pain
If neck pain has a known cause or presents alongside additional symptoms, one of the related ICD-10 codes may be more appropriate.
M54.12 – Radiculopathy, cervical region
Used when neck pain includes nerve root irritation or radiating symptoms into the arm. This code applies when neurological involvement is clearly documented.
M50.20 – M50.23 – Cervical disc displacement
For neck pain associated with disc disorders such as herniation. These codes specify the level and laterality when known.
S13.4XXA – Whiplash injury, initial encounter
Used for trauma-related cervical acceleration–deceleration injuries. This code is appropriate when neck pain results from an acute whiplash event.
R52 – Pain, unspecified
Used when pain is documented but the provider does not specify a location. This should not be used if cervical pain is clearly stated.
When Not to Use ICD-10 Code M54.2
While M54.2 is the standard ICD-10 code for non-specific neck pain, there are several situations where it should not be used because a more accurate or detailed code is required. Using M54.2 incorrectly may lead to claim issues, inconsistent charting, or incomplete clinical documentation.
Neurological deficits are documented
If the patient exhibits numbness, tingling, weakness, or other neurological symptoms, a more specific code such as cervical radiculopathy may be appropriate. These findings indicate that the pain is not simply non-specific but has an identifiable neurological component.
Pain radiates into the arms (suggestive of radiculopathy)
Radiating pain is a red flag that nerve root involvement may be present. In these cases, using a radiculopathy code (e.g., M54.12) provides better clinical accuracy and supports medical necessity for further evaluation.
Trauma, injury, or strain is confirmed
If neck pain results from an accident, fall, lifting injury, or other specific event, trauma-related codes (such as S-codes for injuries or T-codes where applicable) should be used instead of M54.2. These codes reflect the cause and nature of the injury more precisely.
A specific spine disorder is identified
When the provider documents a condition such as cervical disc displacement, stenosis, facet arthropathy, or degenerative disc disease, those diagnosis codes should be used. M54.2 is only appropriate when the pain is non-specific and not linked to a confirmed structural issue.
The provider documents chronic pain without specifying site-specific coding
Chronic pain requires careful coding, and some encounters may call for additional codes such as chronic pain syndrome or chronic pain of the cervical region. If the provider describes the pain as chronic, coders must select the code that best matches the documentation rather than defaulting to M54.2.
Choosing the correct diagnosis code depends entirely on clear provider documentation, ensuring that coding accurately reflects the patient’s condition and clinical findings.
Conclusion
ICD-10 Code M54.2 is the standard ICD-10 code for neck pain, used to document non-specific cervical pain, and it plays a central role in clinical recordkeeping and claims processing across many specialties.
By understanding when to use this code, how to support it with proper documentation, and when alternative ICD-10 codes are more appropriate, providers and billing teams can promote consistency, reduce errors, and support accurate reporting.
This article is for informational purposes only and does not constitute medical, legal, or insurance advice.