High-risk pregnancies require heightened attention, careful coordination, and precise documentation to ensure the best possible outcomes for both mother and baby. In medical coding, accurately capturing this elevated level of care is essential—not only for clinical clarity, but also for compliance, reporting, and reimbursement.
At Healthsure Hub, we help you understand when and how this O09.90 should be applied and how it helps healthcare providers and coding professionals maintain accurate records, support appropriate prenatal monitoring, and align documentation with payer and regulatory expectations.
Overview of O09.90
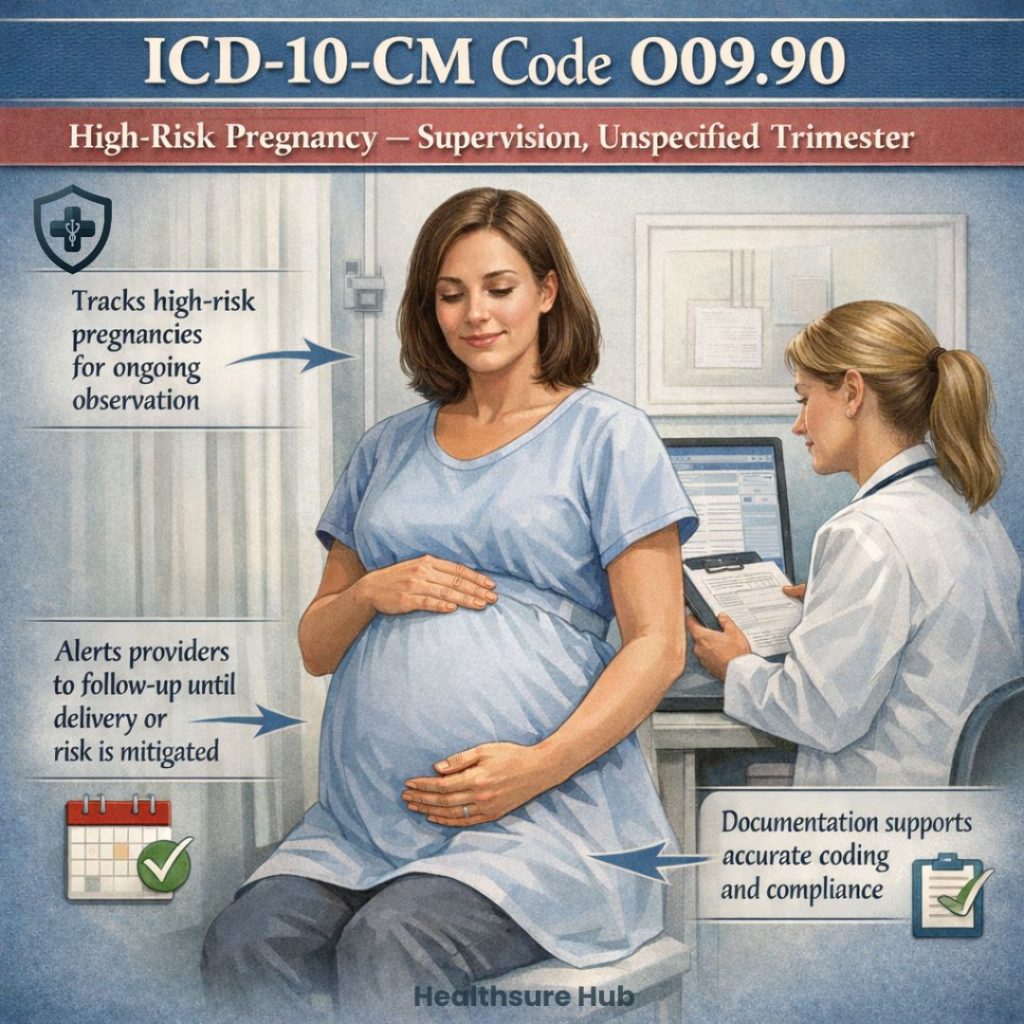
ICD-10 code O09.90 refers to the supervision of high-risk pregnancy, unspecified, unspecified trimester. This code plays a vital role in healthcare documentation, medical billing, and ensuring appropriate care for expectant mothers. Understanding its use, clinical context, and compliance implications is essential for providers, coders, and healthcare administrators.
The code O09.90 is classified under the ICD-10-CM range for supervision of high-risk pregnancies. Each part of the code has a specific meaning:
- Supervision: Indicates ongoing management and monitoring of a pregnancy, rather than treatment of an acute complication.
- High-risk pregnancy: A pregnancy that has an increased chance of adverse outcomes for the mother, fetus, or both. This can include factors such as maternal age, pre-existing medical conditions, multiple gestations, or a history of pregnancy complications.
- Unspecified trimester: The trimester of pregnancy (first, second, or third) is not documented in the clinical record.
This code is designed for situations where the patient is identified as high-risk, but the precise trimester is either unknown or not recorded.
Clinical Context and Common Use Cases
In practice, O09.90 is applied in several scenarios. For example:
- A patient with chronic hypertension or diabetes presents for routine prenatal care, and the healthcare provider documents that the pregnancy is high-risk, but no trimester is specified.
- Early visits to an obstetrician or maternal-fetal medicine specialist before complete gestational information is recorded.
- Situations where risk factors are present, but the focus of the visit is on general supervision rather than treatment of a specific complication.
In some early or uncertain pregnancies, high-risk supervision may also be required when fetal viability cannot be clearly established, which may be documented using ICD-10-CM code O36.80X0. While more specific codes exist for high-risk pregnancies by trimester, O09.90 is often used as an initial or temporary code when documentation does not allow for greater precision.
Differentiation from Related Codes
The ICD-10-CM system includes trimester-specific codes for high-risk pregnancy:
- O09.91: First trimester
- O09.92: Second trimester
- O09.93: Third trimester
These codes are preferred when the trimester is documented, as they provide greater specificity for clinical reporting and insurance purposes. O09.90 serves as a catch-all code when trimester information is missing or unknown, ensuring that the high-risk status is still captured in the medical record.
Importance for Compliance and Reimbursement
Accurate coding is crucial in healthcare for multiple reasons. Using O09.90 appropriately ensures that claims for high-risk pregnancy supervision are processed correctly by insurers. It signals to payers that the patient requires additional monitoring due to elevated risks, which can affect reimbursement rates and resource allocation.
From a compliance standpoint, proper use of O09.90 helps healthcare facilities meet documentation standards and maintain accurate records for audits. While unspecified codes are accepted, overuse without clinical justification may trigger review. Ideally, documentation should eventually allow coders to assign a more specific, trimester-based code.
Documentation Requirements
To support the use of O09.90, medical records must demonstrate:
- Confirmation of high-risk status by a qualified healthcare provider.
- Evidence of ongoing supervision or monitoring throughout the pregnancy.
- Clear documentation if the trimester is unknown or cannot be determined.
Supporting information may include lab results, maternal vital signs, fetal monitoring records, and notes regarding chronic conditions or prior pregnancy complications. Comprehensive documentation not only justifies coding decisions but also promotes optimal patient care.
Epidemiology and Prevalence
High-risk pregnancies represent a significant portion of maternal care. According to studies, approximately 6–8% of pregnancies in the United States are classified as high-risk. O09.90 may be more commonly applied in early or initial visits before complete gestational data is recorded. Patients often fall into high-risk categories due to maternal age (typically over 35), pre-existing health conditions, or multiple gestations.
Clinical Implications
Using O09.90 in patient records carries important implications for clinical care. It alerts providers that the pregnancy requires heightened surveillance, potentially including more frequent prenatal visits, specialized testing, and close monitoring of both maternal and fetal health. The code also supports risk stratification in electronic health records, enabling coordinated care across obstetrics, maternal-fetal medicine, and primary care providers.
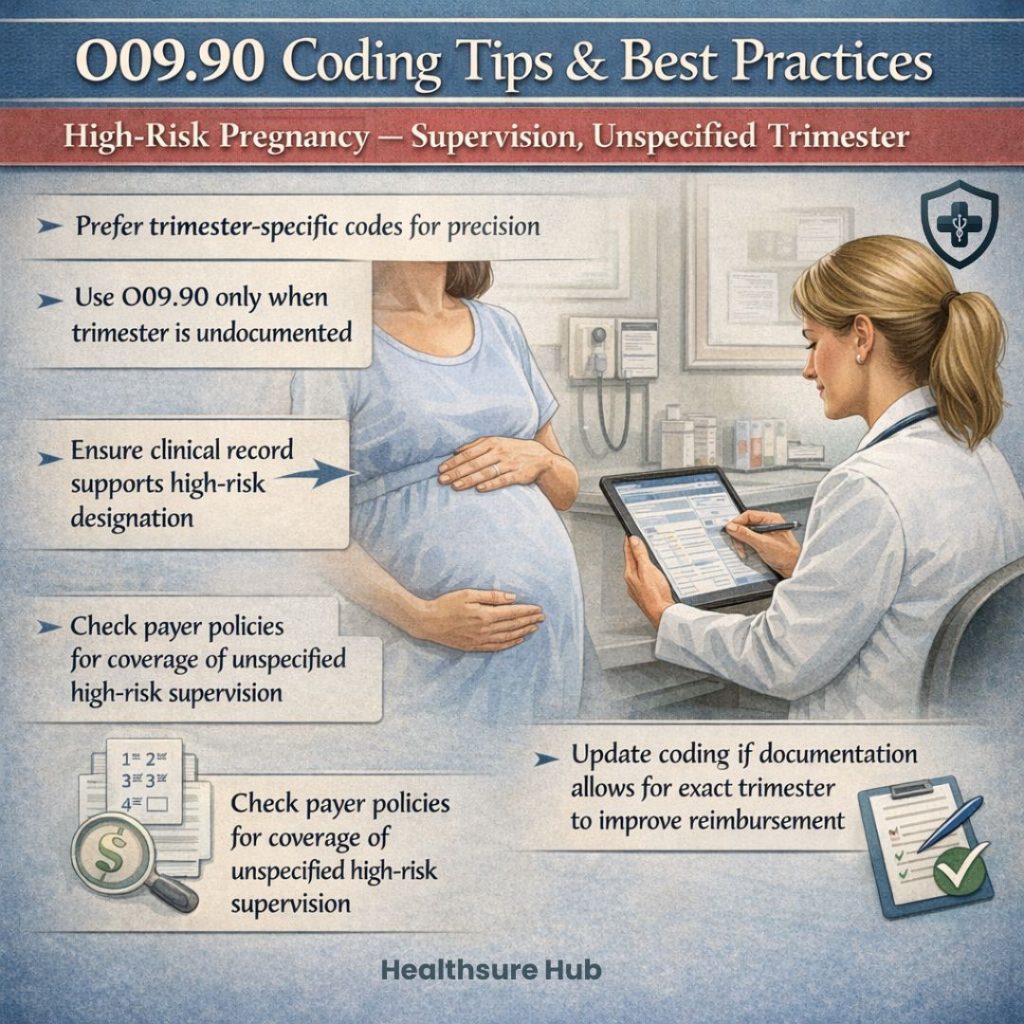
Coding Tips and Best Practices
- Prefer trimester-specific codes when possible to increase precision.
- Use O09.90 only when the trimester is not documented.
- Ensure that the clinical record clearly supports the high-risk designation.
- Review payer policies to confirm coverage for high-risk supervision using unspecified codes.
- Update coding if additional documentation becomes available to reflect the exact trimester, improving reimbursement accuracy.
Conclusion
ICD-10-CM code O09.90 is a critical tool for documenting and managing high-risk pregnancies when the trimester is unspecified. Its proper use ensures that high-risk status is recorded for clinical monitoring, compliance, and reimbursement purposes. While unspecified, the code supports continuity of care and highlights the need for vigilant maternal and fetal surveillance. Ultimately, thorough documentation and timely updates can allow providers to move toward more specific coding, improving both patient outcomes and administrative accuracy.