Pre authorization in medical billing can make or break a healthcare claim—but few really understand why. Behind every denied or delayed payment lies a complex web of insurer rules, clinical documentation, and timing that can leave providers scrambling and patients frustrated. Navigating this hidden process is increasingly tricky, and uncovering how it truly works can mean the difference between smooth reimbursements and costly delays.
What Pre Authorization in Medical Billing Really Means
Pre authorization in medical billing is often referred to interchangeably as “pre‑certification,” “prior approval,” or “predetermination.” All these terms describe the same essential practice: obtaining approval from a health insurance company before moving forward with a service that the insurer considers sensitive, high‑cost, or subject to specific medical necessity rules.
In practical terms, this means that before a provider performs a procedure or orders an expensive medication, the practice must submit documentation, such as CPT and ICD‑10 codes, clinical notes, and justification for the service, to the payer and receive a confirmed authorization. If this step isn’t completed or is done incorrectly, the insurance company may deny or delay the resulting claim, leaving the provider or patient responsible for the cost.

Why Prior Authorization Is Important in Medical Billing
At its best, pre authorization in medical billing protects both insurers and patients from unnecessary costs and inappropriate care. When properly obtained, it helps confirm that a requested service is medically necessary and covered under the patient’s health plan before services are delivered, reducing uncertainty in billing outcomes.
However, pre authorization in medical billing doesn’t just verify coverage. It also:
- Secures revenue and reduces denials – Prior authorization (PA) makes sure that the payer agrees to cover for a service and thus prevents claims denials triggered by missing prior approval. That way it prevents lost revenue for providers.
- Reduces the need for back‑and‑forth appeals or resubmissions – By confirming coverage in advance, PA minimizes the need for time-consuming appeals, claim resubmissions, and administrative follow-ups, streamlining the billing process.
- Prevents fraud – With identity-related insurance fraud projected to rise by 49%, obtaining prior authorization acts as an important checkpoint to detect and prevent fraudulent claims. Incorrect or unnecessary authorization approvals can also lead to overpayment, increasing the risk of payer audits and mandatory refund requests.
- Minimizes unexpected patients out‑of‑pocket expenses – Though often seen as a burden, PA helps confirm coverage upfront, reducing surprise bills and post-service disputes.
Without pre authorization in medical billing, practices risk higher rates of denied or delayed claims, which in turn disrupt accounts receivable and burden administrative teams with costly rework.
How Pre Authorization in Medical Billing Affects Revenue Cycle
Pre authorization in medical billing has a cascading impact on how quickly and accurately providers receive payment, because insurers will not pay (or may reduce payments) for services performed without required prior approval. Many authorization-related errors don’t appear immediately and only surface during the payment posting phase, when payers review claims after reimbursement has already occurred. This influence extends to multiple revenue cycle metrics:
Cash Flow and Accounts Receivable (A/R)
When authorization in medical billing isn’t secured before service, claims can stall or be rejected, often extending accounts receivable aging by 20–30 days on average and creating cash flow bottlenecks. In some cases, claims may be paid but at a reduced rate due to authorization discrepancies, resulting in underpayment that requires additional follow-up and appeals.
Claim Denials and Rejections
Initial denial rates for pre authorization in medical billing takes up for much of the denied claims in medical billing, mostly depending on payer and service type. Many of these denials result from missing documentation, incorrect codes, or mismatched clinical information. Denied or rejected claims directly affect revenue and lead to higher, cost-intensive, appeal rates.
Administrative Costs and Labor Time
Healthcare teams often dedicate extensive staff hours to managing pre authorization in medical billing. Physicians and billers report spending the equivalent of nearly two business days each week just handling these requests, contributing significant administrative overhead.
These delays and resources spent on prior authorizations don’t just cost time—they directly affect a provider’s bottom line through lost productivity, increased operational costs, and delayed collections.
Strategies to Improve RCM Outcomes
While pre authorization in medical billing may greatly affect revenue cycle outcomes there are some possible strategies to improve the RCM outcomes such as:
- Outsourcing PA – Partnering with specialized PA services allows healthcare providers to shift time-consuming administrative tasks to experts. This not only reduces internal staffing costs by up to 70% but also increases approval accuracy, ensuring claims are submitted correctly the first time and minimizing costly denials.
- Automation – Leveraging digital tools and software for PA submissions can dramatically streamline workflows. Automation reduces human errors, speeds up the approval process, and allows staff to focus on more strategic revenue cycle activities, ultimately improving cash flow and operational efficiency.
- Tracking Metrics – Continuously monitoring key performance indicators, such as approval rates, denial rates, and turnaround times, provides critical insights into bottlenecks or recurring issues. By analyzing these metrics, organizations can implement targeted interventions, optimize processes, and enhance overall RCM outcomes.
Common Medical Procedures and Medications That Require Pre Authorization
Pre authorization in medical billing is a critical step for high-cost, high-risk, or frequently overused healthcare services. By obtaining approval in advance, insurers ensure medical necessity, prevent unnecessary spending, and protect patients from surprise bills. Medical procedures and medications that require pre authorization in medical billing are:
Advanced Imaging and Diagnostic Tests
- MRI scans, CT scans, PET scans, nuclear medicine studies, echocardiograms
Why it requires pre authorization
These imaging tests are costly and often requested multiple times. Insurers verify that the procedure is clinically indicated and adheres to evidence-based guidelines before granting approval. Proper documentation, including relevant ICD-10 codes and physician notes, is usually required.
Surgical Procedures
- Spinal surgeries, joint replacements, bariatric surgery, elective orthopedic operations
Why it requires pre authorization
Insurers confirm the procedure’s medical necessity, ensuring it is not experimental, duplicative, or inappropriate. Pre authorization also reduces the likelihood of partial payment or claim denial.
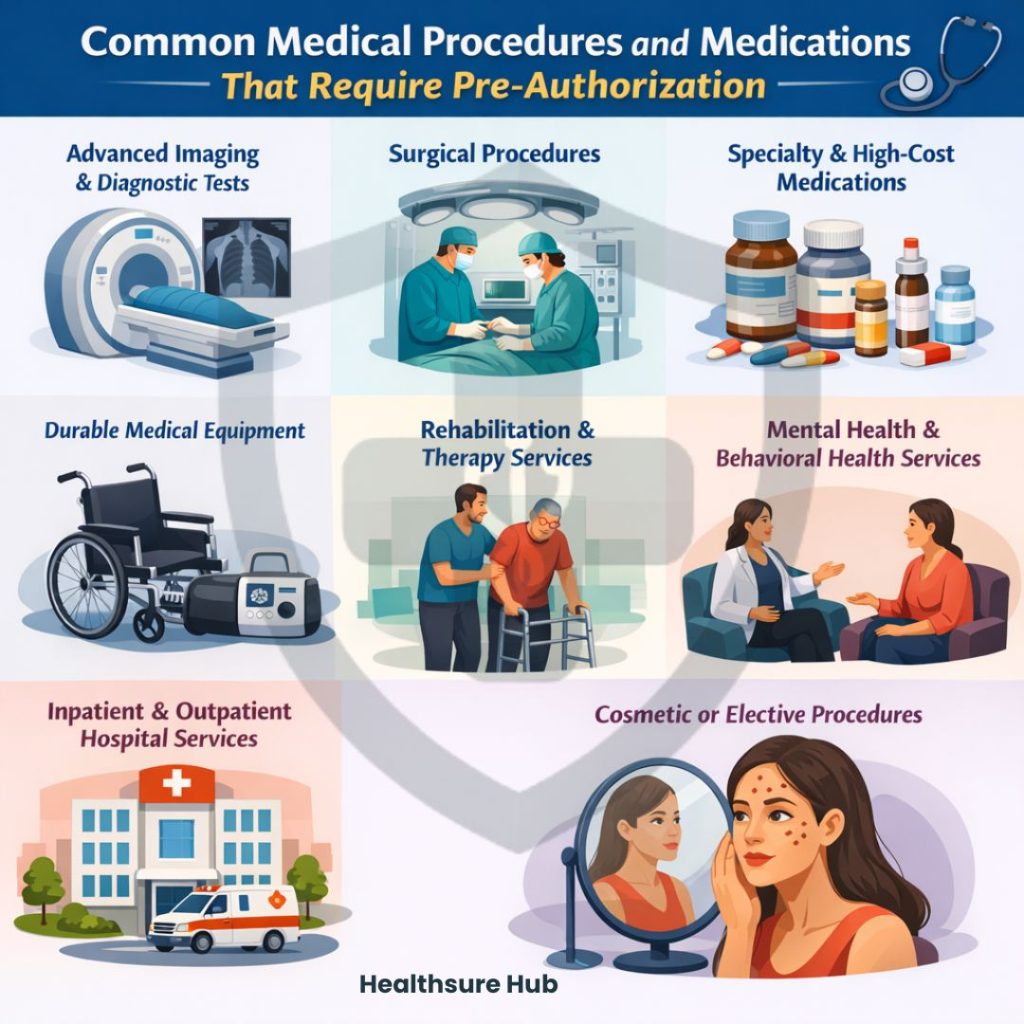
Specialty and High-Cost Medications
- Chemotherapy drugs, biologics for autoimmune conditions, clotting factor treatments, specialty insulin therapies
Why it requires pre authorization
These medications carry significant cost and potential side effects, and may be unsafe when combined with other medication Insurers often require proof that standard therapies have been tried, clinical justification for the drug choice, and detailed prescription documentation.
Durable Medical Equipment
- Wheelchairs, oxygen concentrators, CPAP machines, prosthetics, infusion pumps
Why it requires pre authorization
Pre approval ensures that the equipment is medically necessary, appropriate for the patient’s condition, and meets coverage criteria. This step reduces claim rejections and prevents unexpected out-of-pocket expenses.
Rehabilitation and Therapy Services
- Physical therapy, occupational therapy, speech therapy, cardiac rehabilitation
Why it requires pre authorization
Insurers monitor the number of therapy sessions and their medical appropriateness to prevent overuse. Pre authorization confirms that the therapy aligns with the patient’s diagnosis and documented treatment plan.
Mental Health and Behavioral Health Services
- Inpatient psychiatric stays, outpatient therapy sessions, residential treatment programs
Why it requires pre authorization
These services are frequently high-cost and require careful review to ensure clinical necessity, proper setting, and adherence to treatment protocols. Missing authorization may lead to partial or denied claims.
Inpatient and Outpatient Hospital Services
- Hospital admissions, observation stays, ambulatory procedures, elective inpatient treatments
Why it requires pre authorization
Pre-certification confirms that hospitalization or outpatient procedures are medically necessary and covered under the patient’s plan. It also prevents reduced payment or financial responsibility for patients if coverage rules are not met.
Cosmetic or Elective Procedures
- Rhinoplasty, breast augmentation, laser treatments, cosmetic dermatology procedures
Why it requires pre authorization
Most insurers only cover procedures with a clear medical indication, such as reconstructive surgery after injury or illness. Pre authorization in medical billing helps verify eligibility and avoid claim denials for purely elective services.
How to Request a PA
If your healthcare provider is an in-network provider, they’ll start the pre authorization process. If not, it’s up to you to get approved for pre authorization.
Requesting a pre authorization in medical billing is a structured process that ensures a healthcare service or medication will be covered before it is delivered. The exact steps can vary by insurer and service type, but generally include the following:
- Identify the Need for Authorization
- Collect Required Documentation
- Submit the Request to the Insurance Company
- Receive the Authorization Decision
- Notify the Patient and Schedule Care
How Long It Takes to Get Pre Authorization
While on average it takes 5-10 business days to obtain pre authorization, the timeline depends on multiple factors, including the type of service, insurer policies, and completeness of documentation. Typical timeframes include:
- Standard Services – Routine imaging, lab tests, and therapy sessions may take 2–5 business days for approval.
- High-Cost or Complex Procedures – Surgeries, specialty medications, and inpatient treatments often take 5–14 business days.
- Urgent or Expedited Requests – If a procedure is urgent but not emergent, many insurers offer an expedited review, often completed within 24–48 hours.
Emergency care does not require prior authorization; coverage is determined under emergency provisions.
Conclusion
Pre authorization in medical billing is more than just an administrative step—it is a critical safeguard for both providers and patients. By ensuring that services, procedures, and medications meet medical necessity and payer requirements, prior authorization reduces claim denials, prevents unexpected patient costs, and safeguards revenue. While the process can be time-consuming, understanding and effectively managing pre-authorization is essential for healthcare organizations seeking to maintain financial stability, optimize operational efficiency, and deliver seamless patient care.