In the fast-paced world of healthcare, accurate billing is the lifeblood of any medical practice. One small error in charge posting can delay reimbursements, increase claim denials, and negatively impact cash flow. Every dollar counts, and ensuring that charges are posted correctly is essential for maintaining the financial health of your practice.
We help you understand what charge posting in medical billing is, its importance, cover common challenges, highlight best practices, and explore the benefits of outsourcing charge posting services.
What is Charge Posting in Medical Billing?
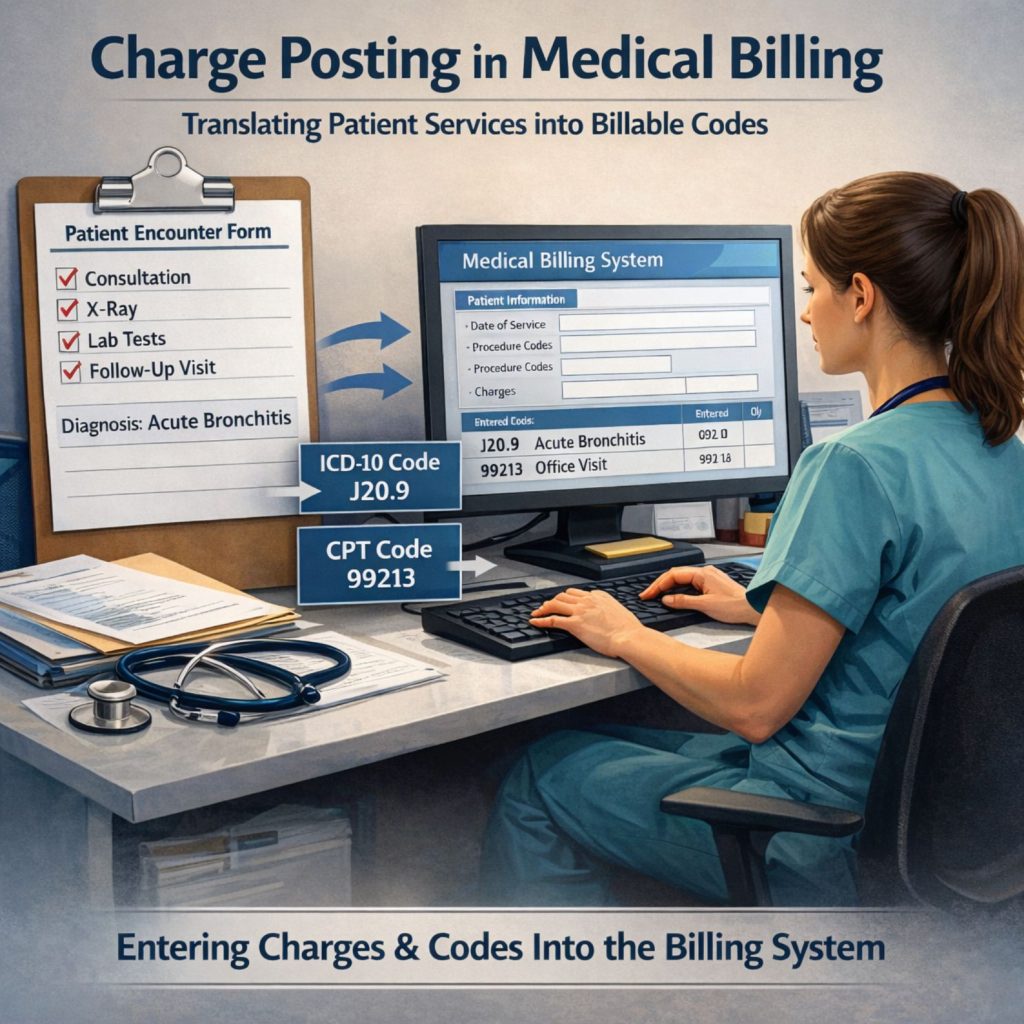
Charge posting in medical billing ,also referred as charged entry, is the step in medical billing where all services provided to a patient are translated into billable codes and entered into the practice’s billing system. These codes include:
- CPT codes (Current Procedural Terminology) – describe the procedures or services performed.
- ICD-10 codes (International Classification of Diseases) – specify diagnoses.
- Modifiers – provide additional information about the service, such as multiple procedures or unusual circumstances.
The process typically starts with a superbill, a detailed document that lists all services provided, their corresponding codes, and associated fees. Charge posting ensures that the information from the superbill is accurately entered into the billing system, which then generates the claims submitted to insurance payers.
If charges are entered incorrectly, claims may be denied, payments delayed, or reimbursement amounts reduced. Accurate charge posting in medical billing is the bridge between patient care and provider revenue.
Why is Charge Posting Important in Medical Billing
Charge posting is more than just data entry but a critical component of the revenue cycle. Here’s why it matters:
- Prevents Claim Denials –Incorrect or missing codes, patient information errors, or improperly applied modifiers are common reasons insurers deny claims. Industry studies show that up to 25% of claims are initially denied due to charge entry errors.
- Speeds Up Reimbursements and Cash Flow –Accurate charge posting allows claims to be processed without delays, ensuring that payments are received faster. Faster reimbursements improve the practice’s ability to pay staff, invest in equipment, and manage operational costs.
- Ensures Compliance – Adhering to HIPAA regulations, CPT/ICD-10 guidelines, and payer-specific rules reduces the risk of audits and penalties. Accurate records demonstrate compliance, protecting the practice from legal and financial consequences.
- Reduces Administrative Burden – Fewer errors mean less time spent correcting claims and handling denials. Staff can focus on patient care and strategic growth rather than chasing unpaid claims.
- Improves Patient Satisfaction – Accurate billing reduces patient confusion and prevents billing disputes, fostering trust in your practice.
Charge Posting in the Medical Billing Workflow
Charge posting in medical billing isn’t just another administrative task, it’s the heart of the medical billing process. Think of it as the bridge between the care your patients receive and the payments your practice needs to thrive. Every accurate entry means faster reimbursements, fewer denials, and a smoother revenue cycle. Understanding each step helps prevent errors and keeps your practice running efficiently. Here’s a step-by-step walkthrough with practical insights and tips:
Patient Registration & Demographics Collection
The journey begins before the first code is even entered. At registration, the front desk collects the patient’s personal information, including:
- Full name and date of birth
- Insurance carrier and policy numbers
- Contact information and preferred method of communication
Why does it matter? Even a small typo can snowball into claim denials or delayed payments. For example, a wrong DOB could prevent the payer from matching the claim to the patient’s policy. As a matter of fact, statistics show that in 2025, almost 50% of claims were denied due to missing or inaccurate claim data.
Common claim denial errors include typos, missing info, outdated insurance, or patients forgetting to update their coverage details. To resolve this it would be best to encourage electronic forms where patients can review their own information, and always double-check insurance details against the payer’s portal. This small step can save hours of back-and-forth later.
Verification of Benefits & Financial Responsibility
Next, the billing team confirms what the patient’s insurance actually covers. This step isn’t just about knowing if a visit is covered, it’s about clarity for both the practice and the patient’s responsibility:
- Does the patient have a copay, deductible, or coinsurance?
- Are certain services excluded or require prior authorization?
- Are there any limits on the number of visits or procedures?
Confirming coverage before services are rendered reduces surprise bills for patients and prevents denied claims due to non-covered services. Common errors include that assuming coverage is standard, miscalculating copays, or missing pre-authorization requirements.
To achieve this, build a routine verification process, ideally integrated into your patient management system, so this step doesn’t fall through the cracks.
Superbill Creation
Once the patient has been seen, the clinician documents all services provided. This information is compiled into a superbill, which is essentially a blueprint for billing.
- Includes CPT (procedures/services), ICD-10 (diagnoses), and any modifiers.
- May also include items like supplies or additional treatments.
Why it matters: The superbill ensures nothing is forgotten. Even one missed service means lost revenue. It’s the foundation upon which the entire claim is built.
Common errors: Missing codes, improperly linking a diagnosis to a procedure, or skipping a service entirely.
Pro tip: Encourage providers to use electronic templates with pre-selected codes for common procedures. It saves time and reduces human error.
Charge Posting / Entry
This is where the magic happens: the charge posting team takes the superbill and enters all the codes and charges into the billing system. Accuracy here is critical. Wrong codes, missing modifiers, or incorrect dates can trigger denials, delayed payments, and extra work.
Common errors:
- Wrong CPT or ICD-10 code
- Incorrect provider or date of service
- Missed modifiers that affect reimbursement
Use double-entry verification or software that flags inconsistencies. Even small details like “place of service” or “modifier usage” can make a difference.
Claim Submission
After posting, claims are submitted electronically, often via a clearinghouse. This ensures that claims are formatted correctly and meet payer requirements.
Why it matters: A claim rejected at submission means delayed payment. Accurate charge posting in medical billing improves first-pass acceptance rates.
Common errors: Incorrect formatting, missing info, or mismatched codes between claim and superbill.
Pro tip: Track which claims get rejected most frequently—patterns can reveal recurring issues to fix upstream.
Claim Adjudication and Adjustments
Once a claim is submitted, the payer reviews it and determines whether to approve it, deny it, or request corrections. This stage is critical because even small mistakes—such as an incorrect CPT code, missing modifier, or mismatched patient information—can lead to delays in reimbursement. Efficient and accurate handling of adjudications ensures that revenue continues to flow smoothly and prevents bottlenecks in the practice’s cash cycle.
Billing teams that track every adjustment and note the reasons for denials or corrections over time gain valuable insights. These records allow staff to identify recurring issues, refine charge posting practices, and ultimately speed up future claims processing. In other words, a well-managed adjudication stage doesn’t just fix errors—it actively prevents them from happening again.
Patient Billing and Statements
After insurance payments are applied, any remaining balance is billed to the patient. Clear and precise patient statements are essential for maintaining trust and ensuring timely payments. Confusing or incomplete bills can frustrate patients, resulting in delays or even disputes over charges.
A best practice is to provide itemized statements that explain each charge in plain language. When patients understand exactly what they are being billed for, they are more likely to pay promptly. Transparency in billing is not just about avoiding errors—it’s a way to enhance patient satisfaction and strengthen the provider-patient relationship.
Follow-up and Appeals for Denied Claims
Denied claims are inevitable, but how they are handled makes all the difference. The billing team must carefully review the denial, correct any errors, and resubmit the claim or file an appeal if necessary. Timely follow-up ensures that denied claims do not linger unpaid, which could otherwise negatively impact revenue and the overall efficiency of the practice.
Maintaining a detailed log of denied claims and the reasons behind each denial is an invaluable tool. Patterns often emerge, revealing systemic issues in coding, documentation, or charge entry. By addressing these root causes, practices can reduce the frequency of future denials and strengthen the overall billing process.
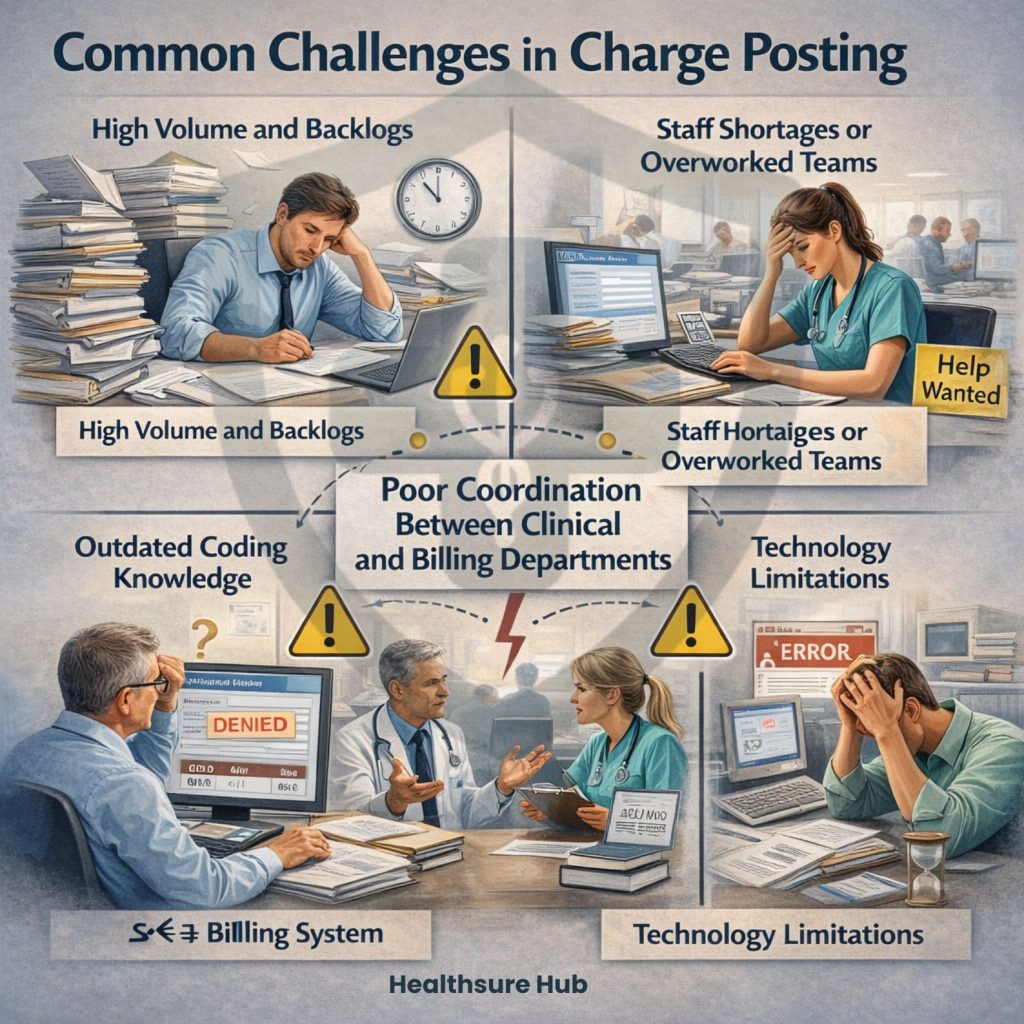
Common Challenges in Charge Posting
Charge posting in medical billing is a critical step, but even seasoned billing teams face multiple challenges that can disrupt the revenue cycle. Understanding these hurdles in depth is key to preventing errors, improving efficiency, and maintaining steady cash flow.
High Volume and Backlogs
Large medical practices, especially those with multiple specialties, often deal with a constant influx of superbills and encounter forms. When these pile up, staff are forced to rush entries, increasing the likelihood of mistakes. Even a small oversight, like entering the wrong procedure code, can lead to upcoding or downcoding that ripple through the entire revenue cycle. Practices experiencing backlogs may also see delays in patient billing, which can frustrate patients and impact cash flow.
Staff Shortages or Overworked Teams
Many practices operate with lean billing teams, relying on a few individuals to manage all incoming charges. Overworked staff are more prone to errors, including incorrect codes, misapplied modifiers, or missing patient details. In some cases, turnover in the billing department exacerbates the problem, as new staff may take time to become familiar with payer-specific rules and workflows. This not only slows down the process but increases the risk of repeated mistakes.
These challenges are becoming more common as the healthcare industry continues to face widespread staffing shortages. Recent healthcare staffing shortage statistics show that administrative and revenue cycle roles are among the hardest to fill, placing even more pressure on already stretched billing teams.
Outdated Coding Knowledge
CPT and ICD-10 codes are updated regularly, and staying current is essential. Staff who haven’t been trained on the latest changes may inadvertently submit claims using obsolete codes. This can trigger denials or audits and even affect compliance with payer and federal regulations. Continuous training and access to updated coding resources are essential to minimize this risk.
Poor Coordination Between Clinical and Billing Departments
Effective charge posting requires seamless communication between providers and billing teams. In many practices, incomplete documentation, unclear notes, or missed entries from the clinical team create bottlenecks. For example, if a clinician fails to note a procedure modifier or documents a service incorrectly, the billing team may submit an inaccurate claim. These miscommunications not only delay reimbursements but also increase administrative burden as claims need corrections.
Technology Limitations
Outdated or poorly integrated billing software can make accurate charge posting in medical billing difficult. Lack of validation tools, slow systems, or software that doesn’t sync with electronic health records (EHRs) can lead to data mismatches, duplicate claims, or lost entries. Practices relying on manual processes are particularly vulnerable, as human error compounds when systems aren’t optimized for efficiency.
Conclusion
Accurate charge posting in medical billing is essential for a smooth revenue cycle, faster reimbursements, and fewer claim denials. By ensuring precise data entry, coordinating with clinical teams, and leveraging technology, practices can protect revenue, reduce administrative burden, and enhance patient satisfaction. Prioritizing efficient charge posting in medical billing not only safeguards compliance but also strengthens the financial health and growth of any medical practice.