Medical billing accuracy is the foundation of a healthy revenue cycle and reliable patient care. When healthcare claims don’t reflect the true services provided, the issues most often involve upcoding and downcoding; two contrasting coding practices that can disrupt finances, compliance, and trust in any medical practice.
Understanding what is upcoding and downcoding, how they occur, and how to prevent them improves billing integrity and strengthens clinical documentation.
What Is Upcoding in Medical Billing?
To understand what is upcoding and downcoding, it’s important to start with upcoding.
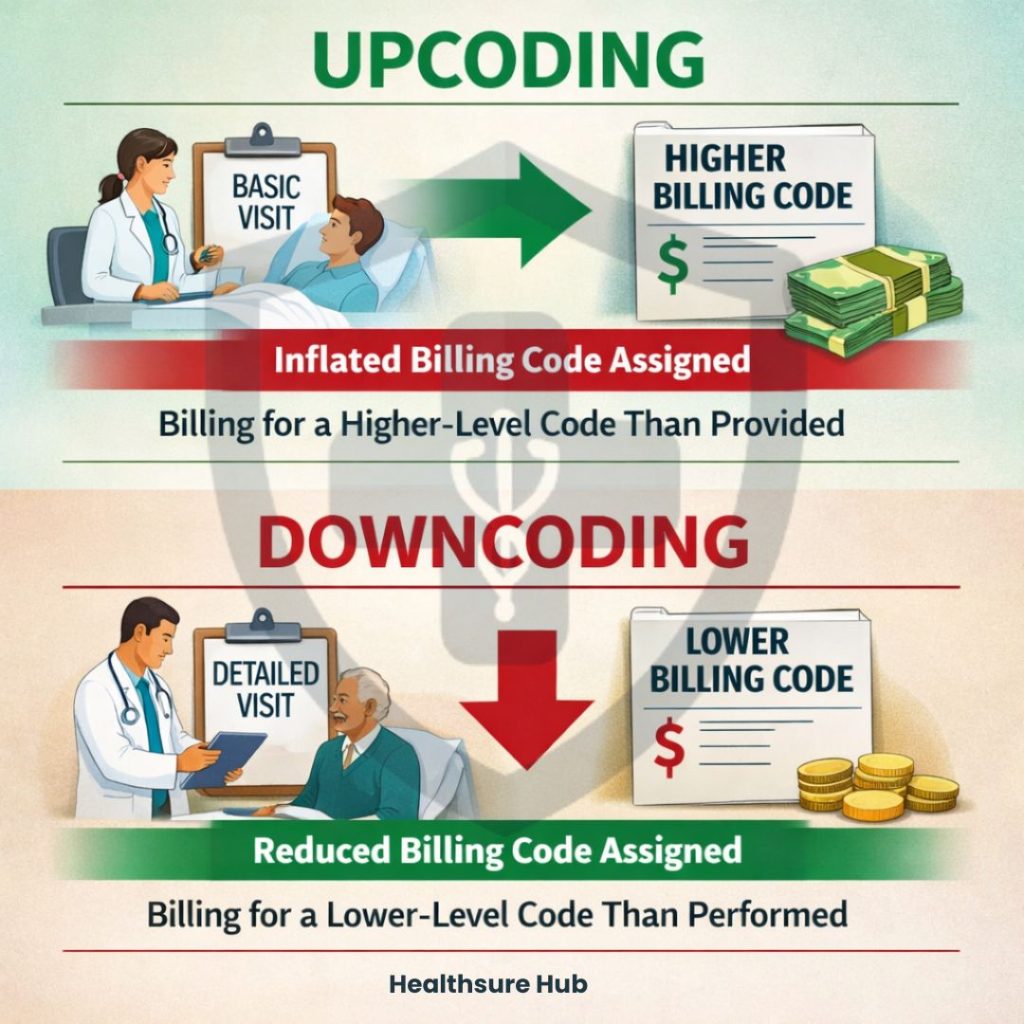
Upcoding is the practice of assigning a higher-level or more complex billing code than what was actually provided or documented. This artificially inflates the reported complexity or scope of the service, which often leads to overpayment from insurers, including private payers and federal programs like Medicare and Medicaid. In essence, upcoding not only misrepresents the care delivered but can also trigger financial and legal consequences due to these improper reimbursements.
In essence, upcoding occurs when the claim reflects a service that appears more resource‑intensive, time‑consuming, or severe than what the clinical record substantiates. In many cases healthcare providers overcharge the patient by assigning a code for a more serious procedure or health issue that the patient has or assigns a service more expensive than what the service provided. This misrepresentation can occur across diagnosis codes, procedural codes, and evaluation and management (E/M) codes, such as billing a Level 4 office visit when documentation supports only a Level 3.
Upcoding is considered fraud when intentional, and even accidental upcoding can trigger audits and penalties if documentation does not support the claim.
Example of Upcoding
Scenario: A 52-year-old male established patient with mild osteoarthritis came in for a routine follow-up because of intermittent knee pain. The physician reviewed his medical record, performed a focused physical examination, and provided lifestyle advice and a minor adjustment to his pain medication. The visit was straightforward, and no imaging or lab tests were required.
Coding and upcoding: The physician spent 15 minutes with the patient and documented a standard evaluation. However, the claim was submitted as CPT code 99214 (moderate-complexity office visit) instead of 99213 (low-complexity visit). This made the visit appear more complex than it actually was, leading to a higher reimbursement than warranted. Because the documentation only supports a low-complexity visit, this is considered upcoding.
How to Spot Upcoded Claims
Practices should:
- Compare payment to what you expected – If a high-level visit or complex service was billed but the reimbursement seems low, it could be downcoded.
- Check the documentation – Make sure the notes support the service level billed. If the documentation shows a higher-level service than what was paid, that’s a red flag.
- Look for patterns – If certain codes are consistently paid at a lower rate, or a particular payer seems to adjust claims more than others, you might be dealing with systemic downcoding.
- Review remittance advice (RA) codes – Codes like CO150 (“information doesn’t support this level of service”) or CARC 186 (“level of care change”) can help identify adjustments.
What Is Downcoding in Medical Billing?
Downcoding is the opposite of upcoding. It’s assigning a lower‑level or less complex code than the level of service that was actually provided and documented by the physician. This leads the physician to receive payments for a lower level of care, than the actual care provided. In practice this leads to reduced reimbursements, because the claim does not fully account for the care delivered, even when the medical record does.
Downcoding may occur when documentation lacks specific details needed to support a higher‑level code, when coding staff choose a conservative code to avoid scrutiny, or when payers themselves adjust codes downward during claims processing.
Unlike upcoding, downcoding is often unintentional and results in financial loss rather than direct legal penalties, though patterns of consistent downcoding can raise compliance issues.
Example of Downcoding
Scenario: A 65-year-old female established patient with type 2 diabetes and hypertension came in for a follow-up after experiencing increased fatigue and occasional dizziness. The physician reviewed her medical record, including recent lab results and medication history, performed a thorough physical examination, measured blood pressure and blood glucose levels, and discussed lifestyle and medication adjustments. A hemoglobin A1c test and basic metabolic panel (BMP) were ordered to monitor her diabetes control. After reviewing the findings, the physician adjusted her medications and provided detailed counseling on diet, exercise, and glucose monitoring.
Coding and downcoding: The physician spent 35 minutes on the encounter and documented high-complexity medical decision-making (MDM), intending to bill CPT code 99214. However, the payer automatically downcoded the claim to 99212, reflecting a lower complexity level. As a result, the provider received a lower reimbursement, even though the care delivered and documentation supported a higher-level service.
How to Recognize Downcoded Claims
As mentioned, downcoding often happens unintentionally, so it’s not always obvious when a claim has been downcoded. To uncover downcoded claims, practices may need to adapt workflows to ensure remittance advice (RA) is reviewed regularly. Working with your EHR or practice management system (PMS) can simplify this process. Many systems allow reporting based on insurance denials or adjustment codes, and your vendor can suggest ways to alert staff when claims are downcoded.
A careful review of remittance advice often reveals downcoding, but not all payers provide clear notifications. Staff may need to compare payments to the expected reimbursement for each CPT code to catch discrepancies. Also, some claims are more prone to being downcoded than others. Tracking claim reductions and denials over time can reveal patterns, helping practices determine whether downcoding is sporadic or consistent with a particular payer, which may indicate a prepayment review program.
What Is Upcoding and Downcoding: Table Comparison
Here’s a simple comparison to understand what is upcoding and downcoding:
| Aspect | Upcoding | Downcoding |
| Definition | Billing for a more complex or costly service than documented | Billing for a less complex or lower‑paid service than documented |
| Primary Result | Increased reimbursement | Reduced reimbursement |
| Common Cause | Intentional fraud or documentation errors | Insufficient documentation, payer edits, defensive coding |
| Legal Risk | High — fraud allegations, fines, audits | Lower, but can trigger audits and compliance issues |
| Impact | Overpayments, risk of enforcement action | Underpayments, revenue loss, audit scrutiny |
| Who Initiates | Provider practice or coder | Payer adjustment or conservative coding |
This table highlights why understanding what is upcoding and downcoding is crucial for compliance and revenue integrity.
Compliance Consequences of Upcoding and Downcoding
Upcoding and downcoding must accurately reflect the services that were actually provided and documented. When coding does not align with the care delivered, it can result in significant financial penalties, audits, and potential legal consequences. According to the General Correct Coding Policies, Chapter 1 issued by the Centers for Medicare and Medicaid Services it clearly states the healthcare providers must avoid downcoding matters as much as upcoding. In the Chapter it clearly states that there’s a HCPCS/CPT code for the services performed, the provider is obliged to report the correct code rather than a similar/more comprehensive describing the services not included in the comprehensive code.
Let’s say that the physician performs a unilateral partial mastectomy with axillary lymphadenectomy, the provider/supplier shall report CPT code 19302, the healthcare provider must report the exact code, not a different one.
The same applies to upcoding. A HSPCS/CPT code must be reported only for the services that have been performed, not for anything else. If a physician performs a unilateral partial mastectomy with axillary lymphadenectomy, the correct code to report is CPT 19302. Reporting any higher-level or different CPT code that represents a more extensive procedure—when that additional service was not actually performed, it refers to upcoding.
When upcoding or downcoding providers may be required to repay improper reimbursements, face financial penalties, or undergo audits and increased scrutiny. In more severe cases, especially involving Medicare or Medicaid, practices may lose the ability to receive reimbursement from public payers altogether.
How to Prevent Upcoding and Downcoding
Preventing upcoding and downcoding requires more than good intentions. It depends on structured documentation, consistent education, and internal oversight that align clinical reality with coding rules. When these elements work together, providers can reduce compliance risk while protecting legitimate reimbursement.
Strong Documentation Practices That Support Accurate Coding
Accurate coding begins with clear, complete, and specific clinical documentation. Every diagnosis, procedure, and level of service must be fully supported by the medical record. When documentation is vague or incomplete, coders may unintentionally select incorrect codes—leading to either upcoding or downcoding.
For example, Evaluation and Management (E/M) codes depend on documented medical decision-making, patient history, and exam complexity. If the documentation does not clearly reflect the true level of service, payers may downcode the claim, or auditors may flag it as potential upcoding.
High-quality documentation should:
- Clearly describe what services were performed
- Match the clinical complexity of the encounter
- Support the exact CPT or HCPCS code reported
- Align with CMS and NCCI documentation requirements
Strong documentation protects providers by ensuring that the codes billed are both accurate and defensible during audits.
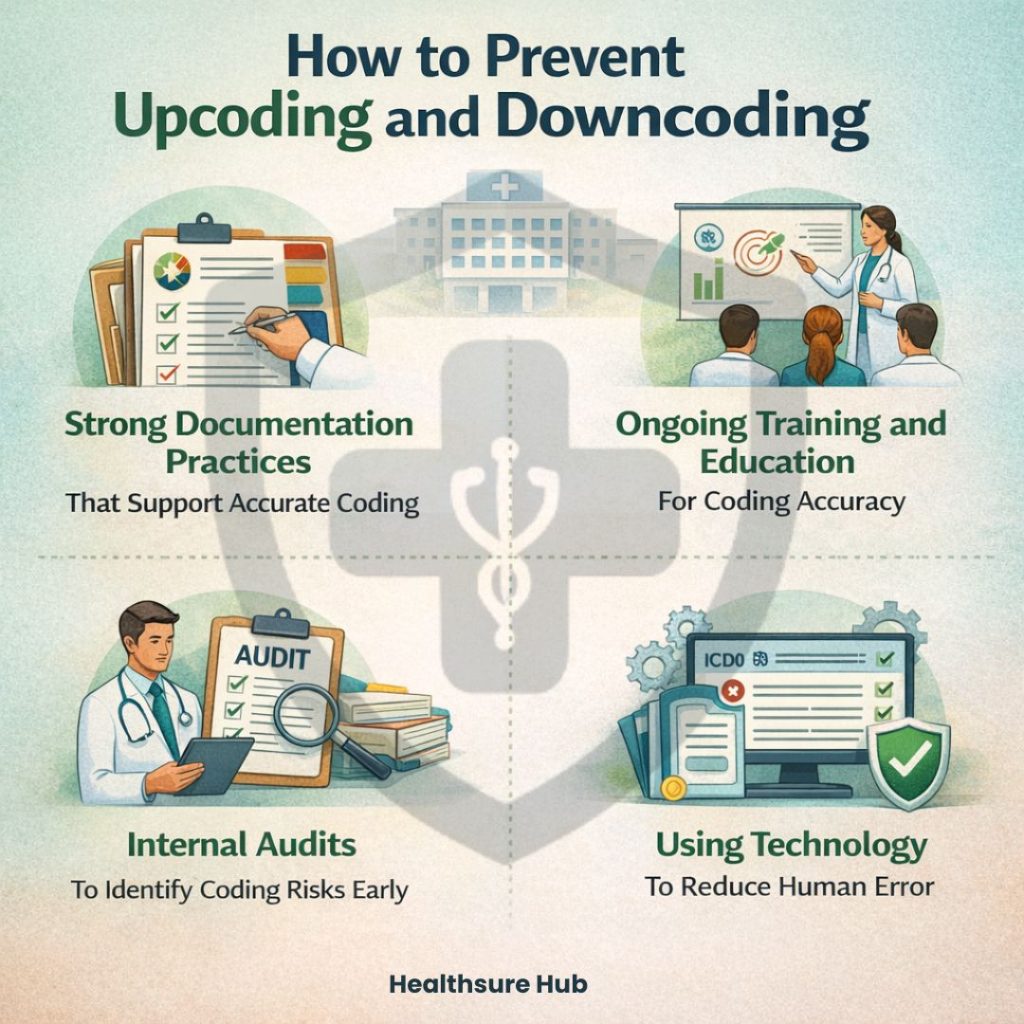
Ongoing Training and Education for Coding Accuracy
Medical coding rules change frequently, especially for E/M services, bundled procedures, and payer-specific edits. Without ongoing education, even experienced coders and providers may apply outdated or incorrect codes, increasing the risk of upcoding and downcoding.
Regular training helps staff:
- Understand current CPT, HCPCS, and ICD-10 guidelines
- Recognize common scenarios that trigger payer downcoding
- Distinguish between legitimate higher-level services and unsupported codes
- Apply NCCI edits and CMS policies correctly
Education should include both clinical staff and billing teams, since documentation and coding decisions are closely linked. Well-trained teams reduce errors before claims are submitted, rather than correcting them after denials or audits.
Internal Audits to Identify Coding Risks Early
Routine internal audits are one of the most effective tools for preventing upcoding and downcoding. By reviewing a sample of claims before or after submission, organizations can detect patterns that may indicate coding inaccuracies.
Internal audits help:
- Identify systematic upcoding or downcoding trends
- Verify that documentation supports billed codes
- Detect payer-specific adjustments or denials
- Correct issues before they escalate into compliance violations
Audits should focus on high-risk services, such as E/M visits, surgical procedures, and frequently downcoded claims. Early intervention reduces repayment demands, audit exposure, and revenue leakage.
Using Technology to Reduce Human Error
Modern coding and billing software can assist in preventing upcoding and downcoding by automatically flagging inconsistencies between documentation and selected codes. These tools apply payer rules, NCCI edits, and coding logic to highlight potential issues before claims are submitted.
Technology can:
- Alert coders to unsupported higher-level codes
- Identify missing documentation that may lead to downcoding
- Reduce manual errors in complex coding scenarios
- Improve consistency across large volumes of claims
While technology does not replace clinical judgment, it serves as an additional safeguard against coding inaccuracies.
Conclusion
Understanding what is upcoding and downcoding is essential for every medical practice. Upcoding occurs when a higher-level service is billed than what was actually provided, while downcoding bills a lower-level service than documented.
Both can hurt revenue and trigger compliance issues. Accurate documentation, ongoing staff training, and smart use of technology are key to preventing these errors and ensuring claims reflect the care actually delivered.