Health insurance is supposed to protect patients, not leave them with surprise bills. Yet millions of Americans are hit with claim denials every year, often for routine or in-network care they assumed was covered. To bring clarity to this growing problem, our team at HealthSureHub analyzed federal Affordable Care Act (ACA) marketplace data, insurer transparency reports, and independent policy studies to uncover which insurance company denies the most claims.
Today, understanding claim denial rates by health insurance companies is just as essential as comparing premiums, deductibles, or copays. Denial rates vary dramatically from one insurer to another, sometimes by hundreds of percentage points, meaning the wrong plan can leave you with thousands of dollars in unpaid medical bills despite being fully insured.
Why Claim Denials Matter More Than Most Consumers Realize
Most people compare health insurance based on three simple numbers: the monthly premium, the deductible, and the copay. But these numbers only tell a part of the entire story.
If an insurer has a pattern of denying a high percentage of claims, your actual out-of-pocket exposure increases dramatically. A plan with a low premium but a high denial rate often turns out to be the most expensive choice in the long run.
This is why getting a glimpse of info about the claim denial rates by health insurance company helps you understand how the effect ripples across your entire healthcare experience. When insurers deny one in four claims, or even one in three, you experience:
- Delays in care
- Unexpected medical bills
- Repeated back-and-forth with providers
- Appeals processes that can take months
- Financial risk even when using in-network doctor

Which Insurance Company Denies the Most Claims?
Based on the most recent ACA marketplace data, a handful of insurers stand out for their significantly higher denial rates. While the exact ranking shifts slightly year-to-year, the same names repeatedly appear at the top of the list.
Oscar Health
Oscar Health has consistently appeared near the top when evaluating which insurance company denies the most claims. In several years of published data, Oscar has denied roughly 25%–26% of all in-network claims. This means one out of every four claims submitted ends in rejection.
Consumers often praise Oscar’s digital tools and customer experience, yet the data shows the company maintains some of the highest denial rates among major national insurers.
Molina Healthcare
Molina Healthcare regularly denies around 22% of in-network claims, placing it well above national averages. Several factors contribute, such as:
- Strict prior authorization requirements
- Narrower provider networks
- Higher administrative denial volumes
For consumers, this combination increases the likelihood of both denied care and denied payment after services are rendered.
Ambetter (Celtic / Centene)
With millions of marketplace enrollees, Ambetter’s national impact is huge. Its denial rates often fall around 20%–21%, which is lower than Oscar or Molina but still significantly above low-denial insurers.
Many consumers report network-access issues and burdensome pre-approval requirements, which align with the elevated denial rate patterns.
UnitedHealthcare
UnitedHealthcare is the largest insurer in the country, and for many years it denied roughly one-third of all marketplace claims. Recent federal transparency data shows a major improvement, with denial rates dropping from 33% to about 19%, but its history of high denials still shapes consumer perceptions.
Even with improvement, UHC remains in the category of insurers with higher-than-average claim rejections.
Which Insurers Deny the Fewest Claims? The Low-Denial Performers
On the opposite end of the spectrum are insurers with consistently low denial rates — some rejecting only 1–6% of claims. These companies tend to have strong administrative systems and more predictable underwriting practices.
Kaiser Permanente
Kaiser consistently denies 6% or fewer in-network claims, making it one of the strongest performers nationally. Its integrated model — where insurance and medical care are part of the same organization — contributes to fewer administrative errors and clearer care pathways.
Providence, Avera, and Sanford Health Plans
Several regional insurers, including Avera and Sanford, maintain denial rates between 1% and 5%, making them some of the most reliable in terms of claims payment processing.
These companies may not operate nationally, but in the states where they are available, they offer some of the lowest denial risks.
State-Level Differences in Denial Rates
Denial rates vary by more than 500% depending on your state.
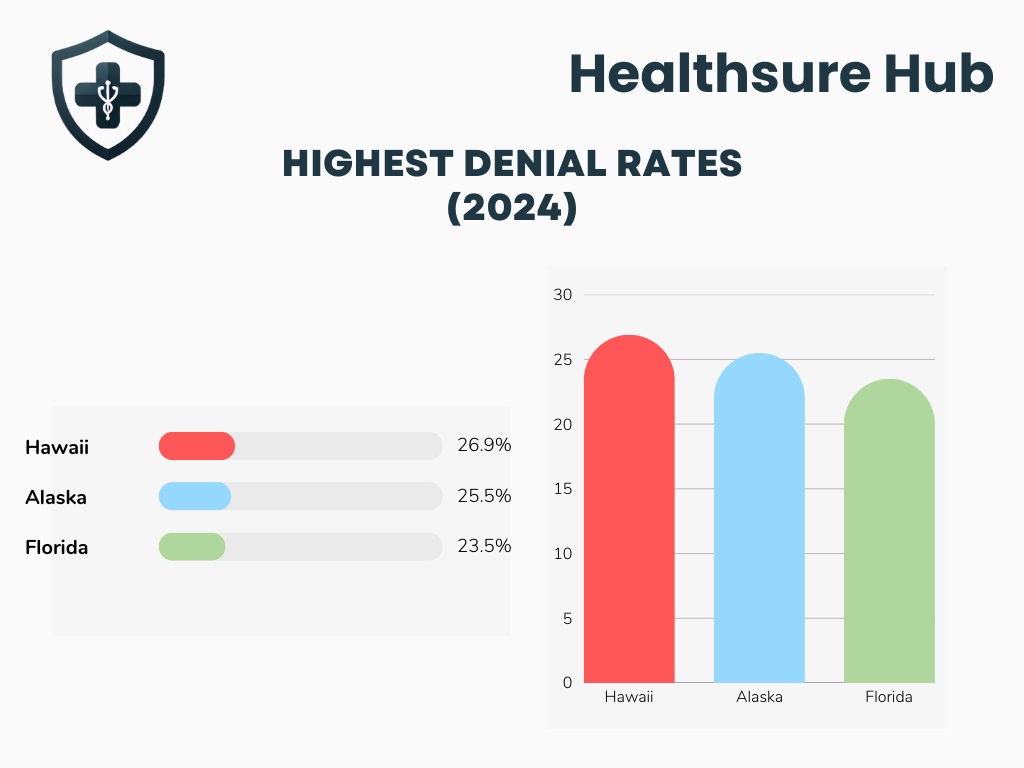
Highest Denial Rates (2024):
- Hawaii – 26.9%
- Alaska – 25.5%
- Florida – 23.5%
Lowest Denial Rates (2024):
- South Dakota – 5.4%
- North Dakota – 9.7%
- Montana – 12.2%
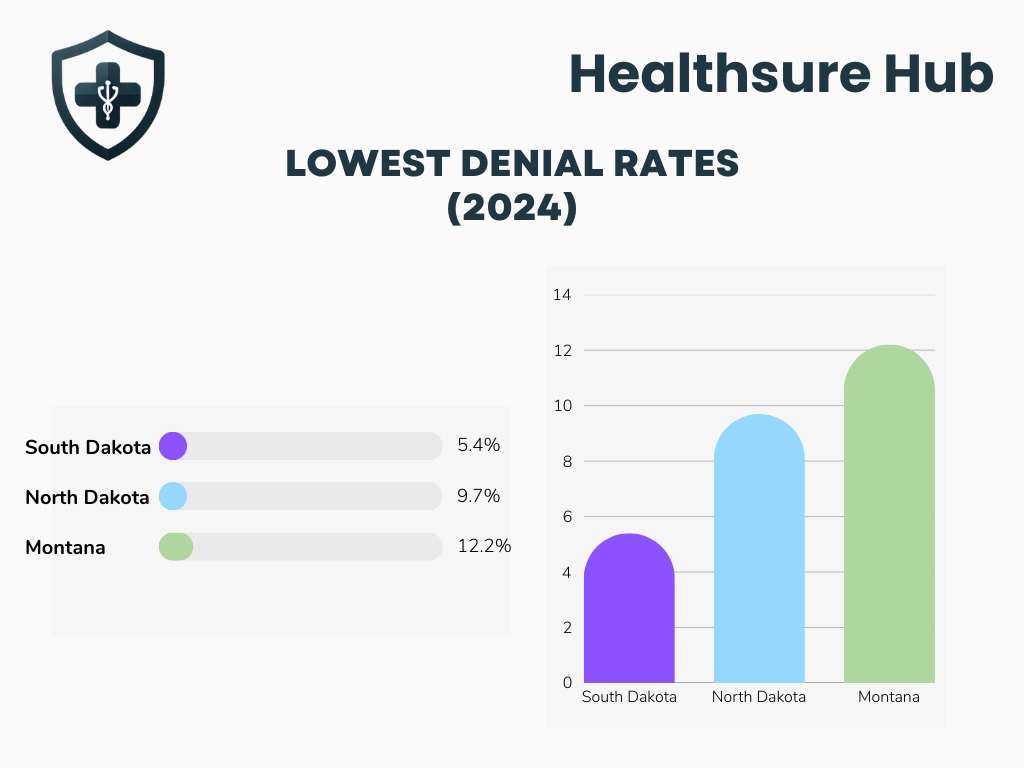
This is why national lists of which insurance company denies the most claims don’t tell the full story, some insurers deny far more in certain regions.
The Real Causes Behind Rejected Claims
When examining claim denial rates by health insurance company, one theme becomes clear: most denials have nothing to do with medical necessity.
In fact:
- 40% are administrative
- 25% are coverage or eligibility issues
- 12% involve prior authorization
- 7% + 2% are medical necessity denials (non-behavioral and behavioral)
Even the most diligent consumer cannot fully control these factors. This is precisely why the insurer you choose — and its behavior — matters so much.
Conclusion
After reviewing federal ACA data, transparency filings, and policy research, one thing that remains clear is that claim denial rates by health insurance company vary dramatically, and those differences can determine whether you feel protected or financially exposed.
Insurers like Oscar Health, Molina Healthcare, Ambetter, and UnitedHealthcare frequently appear near the top of lists identifying which insurance company denies the most claims, while organizations such as Kaiser Permanente and several smaller regional plans consistently demonstrate much lower denial behaviors.
Sources:
https://www.kff.org/private-insurance/claims-denials-and-appeals-in-aca-marketplace-plans-in-2023/
https://www.moneygeek.com/insurance/health/aca-claim-denial-rates-by-state-and-insurer/
https://www.valuepenguin.com/health-insurance-claim-denials-and-appeals
https://www.techtarget.com/revcyclemanagement/feature/Breaking-down-claim-denial-rates-by-healthcare-payer