Medical billing codes often feel cold and technical, but the care behind them is anything but. When patients see CPT code 99401 on a medical bill or insurance statement many are left wondering about the service billed.
CPT 99401 code represents something fundamental to modern healthcare that is preventive counseling. It covers the time a healthcare provider spends educating, guiding, and empowering a patient to make healthier choices before illness develops. Understanding this code helps patients feel more confident about their care, and helps providers and billers ensure services are documented and reimbursed correctly.
Our team at Healthsure Hub explains CPT 99401 clearly, without jargon, so anyone reading it can understand what it means and why it matters.
What Is CPT Code 99401?
CPT code 99401 is used to bill preventive medicine counseling or risk factor reduction interventions provided to an individual patient.
It refers to one-on-one counseling focused on preventing future health problems, rather than diagnosing or treating a current condition. The service is typically face-to-face and lasts approximately 15 minutes.
Unlike many medical codes, CPT 99401 is not tied to a specific illness. Instead, it focuses on education, behavior change, and health awareness which are the building blocks of preventive care.

What Does CPT Code 99401 Actually Cover?
CPT 99401 covers counseling that helps patients reduce health risks and improve long-term well-being. The counseling must be preventive in nature, meaning it is not primarily aimed at treating an existing disease. Common topics include:
- Nutrition and healthy eating habits
- Physical activity and exercise guidance
- Tobacco use prevention or cessation counseling
- Alcohol or substance misuse education
- Sexual health and safe practices
- Stress management and mental wellness
- Injury prevention and safety education
What matters most is not the topic itself, but the intent of the service. The goal must be to prevent illness or reduce risk, not to manage an already-diagnosed condition.
Who Can Receive Services Billed Under CPT Code 99401?
Preventive counseling is not limited to a narrow group of patients. CPT 99401 may be used for:
- Adults who are generally healthy but have risk factors
- Adolescents and young adults receiving health education
- Patients with a family history of chronic disease
- Individuals seeking guidance after screenings or lab results
- People making lifestyle changes to improve overall health
A patient does not need to be “sick” for CPT 99401 to apply. In fact, the code is specifically designed for patients before a diagnosis exists, when education can have the greatest impact.
Who Can Bill CPT Code 99401?
CPT 99401 code may be billed by qualified healthcare professionals, including:
- Physicians
- Nurse practitioners
- Physician assistants
- Other licensed providers, depending on payer rules
The service is commonly delivered in:
- Primary care practices
- Preventive health visits
- Community health clinics
- Outpatient settings
In some cases, CPT 99401 may also be reimbursed for telehealth visits, provided payer requirements are met and documentation supports the service.
CPT Code 99401 vs Other Preventive Counseling Codes
CPT 99401 is part of a family of preventive counseling codes that differ based on time:
- 99401 – Approximately 15 minutes
- 99402 – Approximately 30 minutes
- 99403 – Approximately 45 minutes
- 99404 – Approximately 60 minutes
Providers must select the code that best reflects the actual time spent counseling the patient. Choosing a higher-level code without proper time documentation can lead to claim denials or audits.
Documentation and Time Requirements for CPT Code 99401
Proper documentation is essential when billing CPT Code 99401. Because this code is time-based and preventive, insurers closely review whether the service was clearly supported in the medical record.
Documentation should include:
- The preventive topic(s) discussed (such as nutrition, exercise, or risk reduction)
- The reason counseling was appropriate, including risk factors or preventive intent
- The total time spent providing counseling (typically about 15 minutes)
- Evidence of direct, individual interaction with the patient
Time must be explicitly documented. Vague statements such as “discussed lifestyle changes” without a time reference are a common reason for claim denial. Clear, specific documentation helps demonstrate that the counseling was medically appropriate and distinct from other services provided during the visit.
CPT 99401 vs Office Visit (E/M) Codes
CPT 99401 code is different from standard evaluation and management (E/M) office visit codes. While office visits focus on diagnosing symptoms and managing medical conditions, CPT 99401 is used specifically for preventive counseling and education.
In some situations, CPT 99401 may be billed during the same encounter as an office visit. This is only appropriate when:
- Preventive counseling is separate and distinct from the problem-focused visit
- Both services are clearly documented
- The preventive counseling includes its own time and purpose
When billed together, insurers may require a modifier to indicate that preventive counseling was not bundled into the office visit. Failure to clearly separate these services is a common cause of denied or reduced reimbursement.
Insurance Coverage and Reimbursement Considerations
Coverage for code 99401 CPT varies by insurer. Some health plans actively support preventive counseling, while others apply restrictions based on:
- Patient age
- Risk factors
- Frequency limits
- Network status
Medicare and Medicaid policies differ from commercial plans, and not all preventive counseling services are automatically covered. Even when counseling is medically appropriate, claims may be denied if payer-specific requirements are not met.
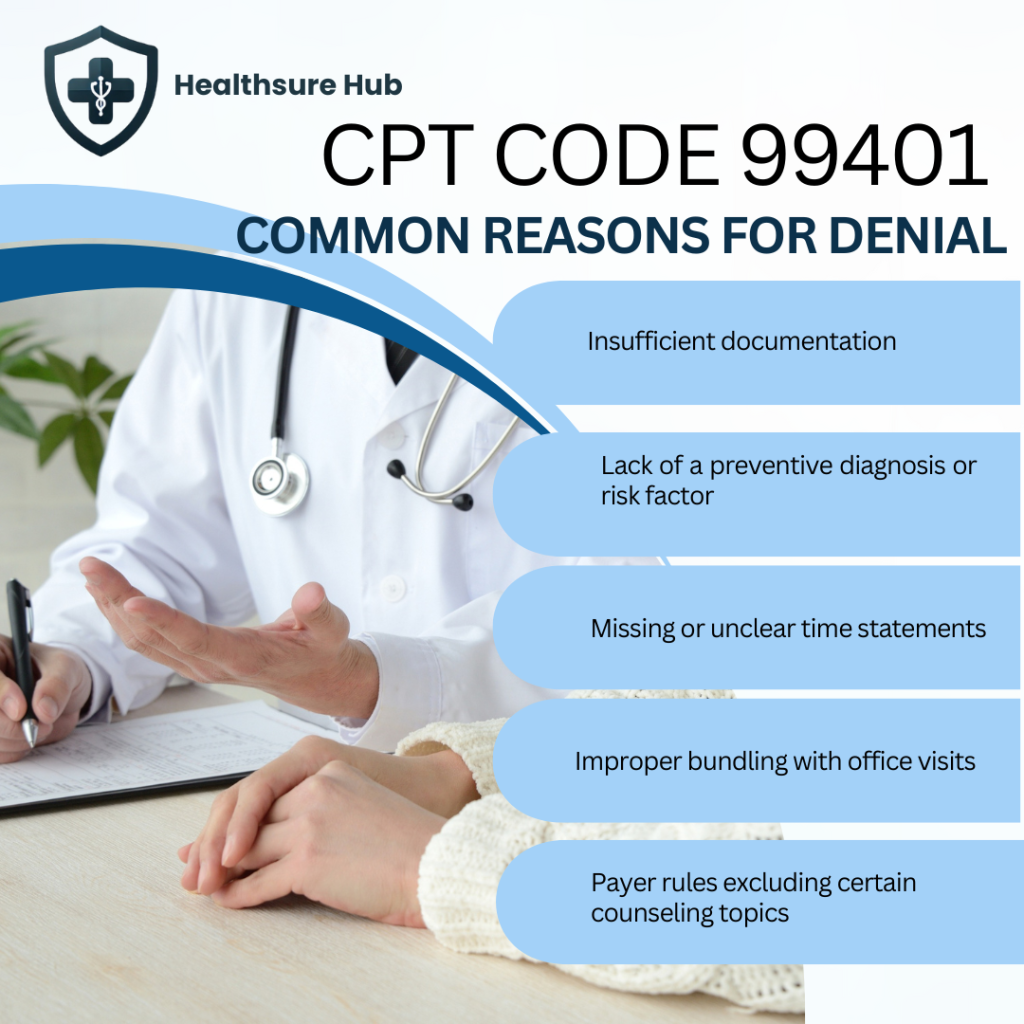
Common Reasons CPT 99401 Code Is Denied
Despite being a legitimate preventive service, CPT 99401 is often denied due to:
- Insufficient documentation
- Lack of a preventive diagnosis or risk factor
- Missing or unclear time statements
- Improper bundling with office visits
- Payer rules excluding certain counseling topics
Understanding these pitfalls helps providers improve billing accuracy and helps patients understand why a charge may appear or be rejected.
Conclusion
99401 CPT represents meaningful time spent helping patients make healthier choices. It applies to preventive counseling, not treatment, and requires clear documentation and appropriate timing.
For patients, understanding this code brings clarity to medical bills. For providers and billers, it ensures preventive care is accurately reported and supported.
When used correctly, CPT Code 99401 reflects the growing importance of prevention in modern healthcare while helping people stay healthy, not just get treated.