Denied claims are a persistent and costly challenge for healthcare providers. Every year, hospitals in the U.S. lose an estimated $262 billion due to claim denials, with many of these losses avoidable through effective denial management in healthcare.
Our team at Healthsure Hub helps you understand why denial management in healthcare is critical for any provider seeking to improve financial performance, reduce claim rework, and maintain compliance with payer requirements.
What is Denial Management in Healthcare
Denial management in healthcare is the organized process of identifying, analyzing, resolving or preventing claims that have been denied, postponed or lost. It is both operational and strategic, combining technology, staff expertise, and workflow optimization to maximize revenue recovery and reduce administrative burden.
A claim denial occurs when a payer, such as an insurance company or government program, refuses to pay for a service rendered. Denial management in healthcare encompasses four key activities:
- Detecting denied claims early in the revenue cycle.
- Analyzing the reasons behind denials.
- Reworking or appealing claims to recover payment.
- Implementing preventive measures to minimize future denials.
Unlike simple claim correction, denial management is proactive, aiming to identify patterns, improve workflows, and reduce recurring errors. It involves multiple departments, including billing, coding, clinical staff, and revenue cycle management teams, and relies heavily on integrated technology solutions to streamline operations.

Why Denial Management Is Critical
Claim denials are costly in both time and resources. According to claim denials statistics:
- Four in ten providers report that at least 10% of their claims are denied.
- 90% of denials require human review to resolve.
- 41% of providers say that at least one out of every ten claims they submit ends up denied.
Denied claims delay revenue, increase administrative workload, and disrupt cash flow. For understaffed organizations, even minor inefficiencies can accumulate into significant financial loss. Effective denial management in healthcare improves operational efficiency, ensures compliance, and protects patient satisfaction by enabling accurate, timely billing.
Additionally, 60–65% of denied claims are potentially recoverable. This highlights that denial management is not just an administrative necessity but a revenue preservation strategy. Practices that implement structured denial management processes can reclaim significant lost revenue and reduce the risk of repeated denials.
Denial management is one component of revenue cycle integrity, alongside managing overpayments, underpayments, and post-payment reviews. Together, these processes ensure that providers not only receive the correct reimbursement but also minimize financial losses across the revenue cycle.
Common Causes of Medical Billing Denials
Denials occur for many reasons, and understanding the root cause is essential for prevention. Common causes include:
- Coding Errors – Incorrect or mismatched CPT, HCPCS, or ICD codes are a leading cause of denials. Even minor inaccuracies can result in claim rejection.
- Missing Documentation – Claims submitted without required documentation, such as operative notes or prior authorizations, are frequently denied.
- Eligibility Issues – Patients whose insurance coverage has expired or is inactive at the time of service may trigger a denial.
- Prior Authorization Gaps – Services requiring pre-approval can be denied if authorization is missing, incomplete, or expired
- Medical Necessity Disputes – Claims may be rejected if the payer determines that the service is not medically necessary.
- Duplicate Claims– Submitting multiple claims for the same service leads to automatic denials.
By categorizing denials by type, payer, and service line, organizations can identify patterns and implement corrective actions. Root cause analysis allows providers to address systemic issues rather than continuously reworking the same errors, which is central to denial management in healthcare.
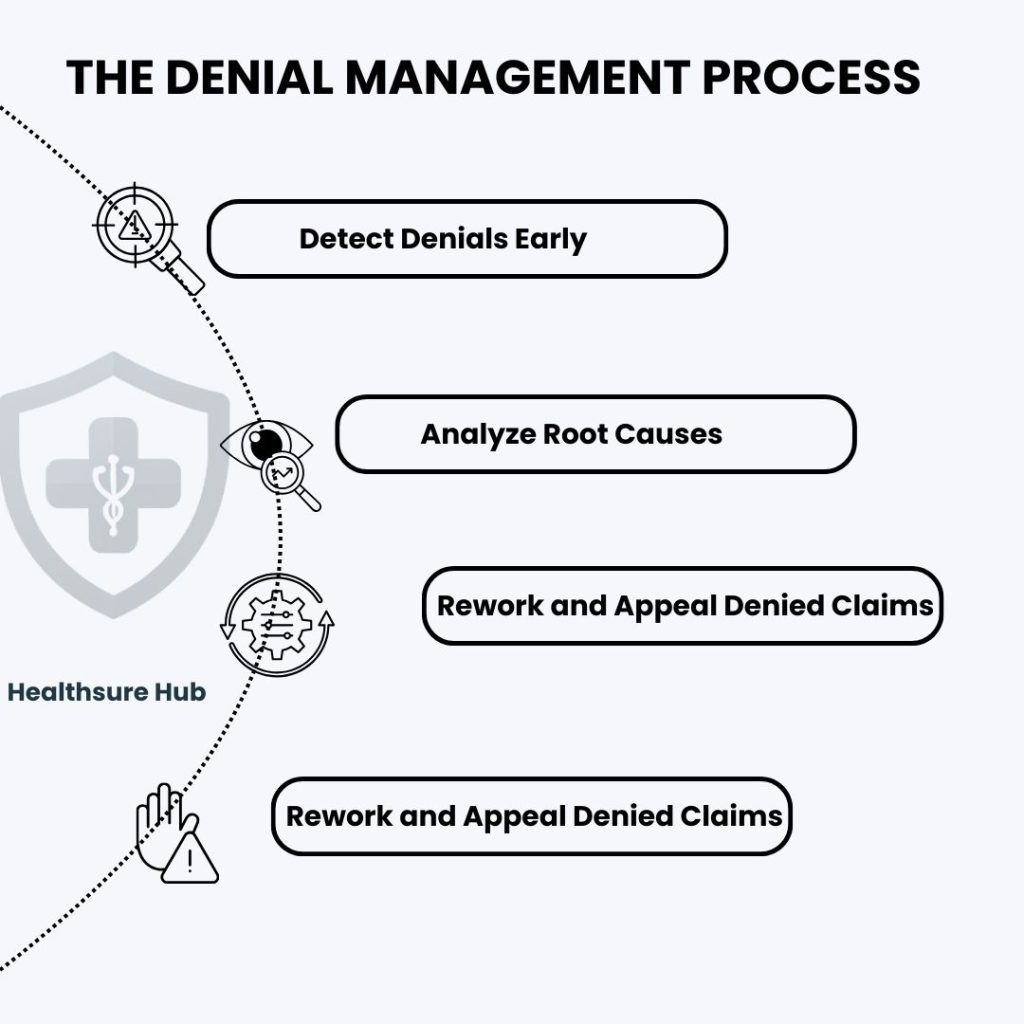
The Denial Management Process
A structured approach ensures that denials are addressed efficiently and consistently. There are several steps to take to ensure successful denial management including:
Detect Denials Early
Early detection is critical for timely resolution. Claims should be monitored from submission to adjudication using tools like Explanation of Benefits (EOBs), Electronic Remittance Advice (ERA) statements, and automated claims dashboards. Most states, including the State of Michigan, require that claims are paid within 30 to 45 days.
To detect denied claims practices need to run reports on claims that exceed the maximum 45 days period and ask for the status of the claim. Detection involves categorizing claims by payer, denial reason, service type, and department. Automated dashboards can flag high-risk claims immediately, reducing the time between denial receipt and rework. By detecting denials early, providers increase the likelihood of successful recovery and minimize revenue delays.
Analyze Root Causes
Once a denied claim is identified, the next step is to determine why. Root cause analysis is essential to identify recurring issues, whether they relate to coding errors, documentation gaps, duplicate claims, eligibility, or authorization issues.
High-volume denials should be tracked to identify trends. For example, if multiple claims for a specific procedure code are denied due to missing documentation, staff training or workflow adjustments can prevent future denials. Categorizing and analyzing denials also helps in prioritizing claims for rework and appeal, focusing resources on high-value opportunities, a strategy central to denial management in healthcare.
Rework and Appeal Denied Claims
Reworking denied claims is labor-intensive but critical for revenue recovery. It involves:
- Gathering and correcting missing documentation
- Updating coding errors
- Resubmitting corrected claims to payers
- Filing appeals when necessary
Appeals may follow payer-specific guidelines or standardized processes like the CMS five-level Medicare appeal process. Prioritization is essential; high-value claims or those with a high likelihood of recovery should be addressed first. Efficient rework workflows reduce turnaround time and increase revenue capture, which is a hallmark of effective denial management in healthcare.
Prevent Future Denials
Prevention is the most effective strategy for managing denials. Steps include:
- Staff Training – Keep billing and coding staff updated on regulations, payer requirements, and documentation standards.
- Workflow Improvements – Implement front-end registration checks, prior authorization verification, and eligibility verification to reduce errors before claims are submitted.
- Technology Integration – Utilize practice management systems, EHR integration, and automated claim validation tools.
- AI-Powered Predictive Analytics – Predictive algorithms can flag high-risk claims before submission, enabling proactive intervention.
- Continuous Monitoring – Track key performance indicators (KPIs) like first-pass clean claim rate, denial resolution time, and recovery percentage to identify areas for improvement.
Preventive measures reduce both the number of denials and the cost of rework, ultimately improving cash flow and operational efficiency.
The Role of Technology in Denial Management
Technology is the backbone of modern denial management. Integration of practice management systems and electronic health records allows for real-time claim validation and error detection, ensuring that claims submitted are clean and compliant.
AI-powered solutions take denial management further by predicting which claims are at risk for denial, enabling proactive intervention. Automation minimizes manual errors, accelerates appeals, and provides data visualization for trend analysis, root cause identification, and compliance audits. Organizations that adopt these technologies typically experience reduced denial rates, faster claim resolution, and improved operational efficiency.
Denial Management Strategies
Effective denial management in healthcare requires a combination of human expertise and technological support:
- Staff Education and Accountability – Training staff on coding updates, documentation requirements, and payer policies reduces human error. Establishing clear accountability for denial resolution ensures that claims are addressed efficiently.
- Workflow Optimization – Streamline processes for claim submission, verification, and documentation. Front-end registration checks and prior authorization workflows reduce preventable denials.
- Technology and Automation – Modern practice management systems and EHR integration allow real-time error detection, automated workflows, and integrated documentation. AI-driven predictive analytics can identify high-risk claims, prioritize high-value cases for human intervention, and minimize unnecessary rework.
- Continuous Performance Monitoring – Track denial trends and root causes through dashboards. Regularly review key metrics and implement corrective actions to maintain improvement.
By combining these strategies, organizations can reduce denial frequency, shorten resolution time, and maximize revenue recovery.
Measuring Success in Denial Management
Success in denial management in healthcare can be quantified through specific KPIs:
- First-Pass Clean Claim Rate – The percentage of claims approved without rework.
- Denial Resolution Time – Average time taken to resolve denied claims.
- Recovery Rate – The proportion of denied claims successfully recovered.
- Denial Rate by Cause – Categorization by type helps target preventive actions.
Monitoring these metrics enables organizations to refine workflows, train staff more effectively, and improve revenue cycle performance.
Conclusion
Denial management in healthcare is a critical, data-driven component of revenue cycle management. By detecting, analyzing, reworking, and preventing denied claims, healthcare providers can safeguard revenue, reduce administrative burden, and improve operational efficiency.
Integrating staff training, workflow optimization, technology solutions, and AI-driven predictive analytics allows practices to minimize denials before they occur and maximize recovery when they do. In a competitive healthcare environment where cash flow and operational efficiency are vital, effective denial management in healthcare is not optional, it is essential.