Healthcare staffing shortage statistics reveal more than hiring challenges, they expose how workforce gaps shape patient outcomes, hospital readmission rates, access to care, and system sustainability. In 2025, staffing shortages remain one of the most measurable and solvable pressures facing healthcare systems, making accurate data essential for understanding what comes next.
This evidence-based analysis consolidates the most important healthcare staffing shortage statistics, explains what they mean in real-world settings, and connects workforce capacity directly to quality, safety, and continuity of care. Our team at Healthsure Hub dived deep into research, peer-reviewed studies, national workforce datasets, and healthcare system reports to identify the trends that matter most for providers, patients, and policymakers.
Top Healthcare Staffing Shortage Statistics You Need to Know
- The U.S. healthcare system is projected to face a physician shortage of up to 187,130 full-time equivalent physicians by 2037, driven by retirements and rising patient demand.
- An estimated one million nurses are expected to retire between 2027 and 2030, removing decades of clinical experience from hospitals and care facilities.
- The number of licensed RNs reached 5.86 million in 2025.
- The annual salary for a registered nurse is $94,480 as of 2025.
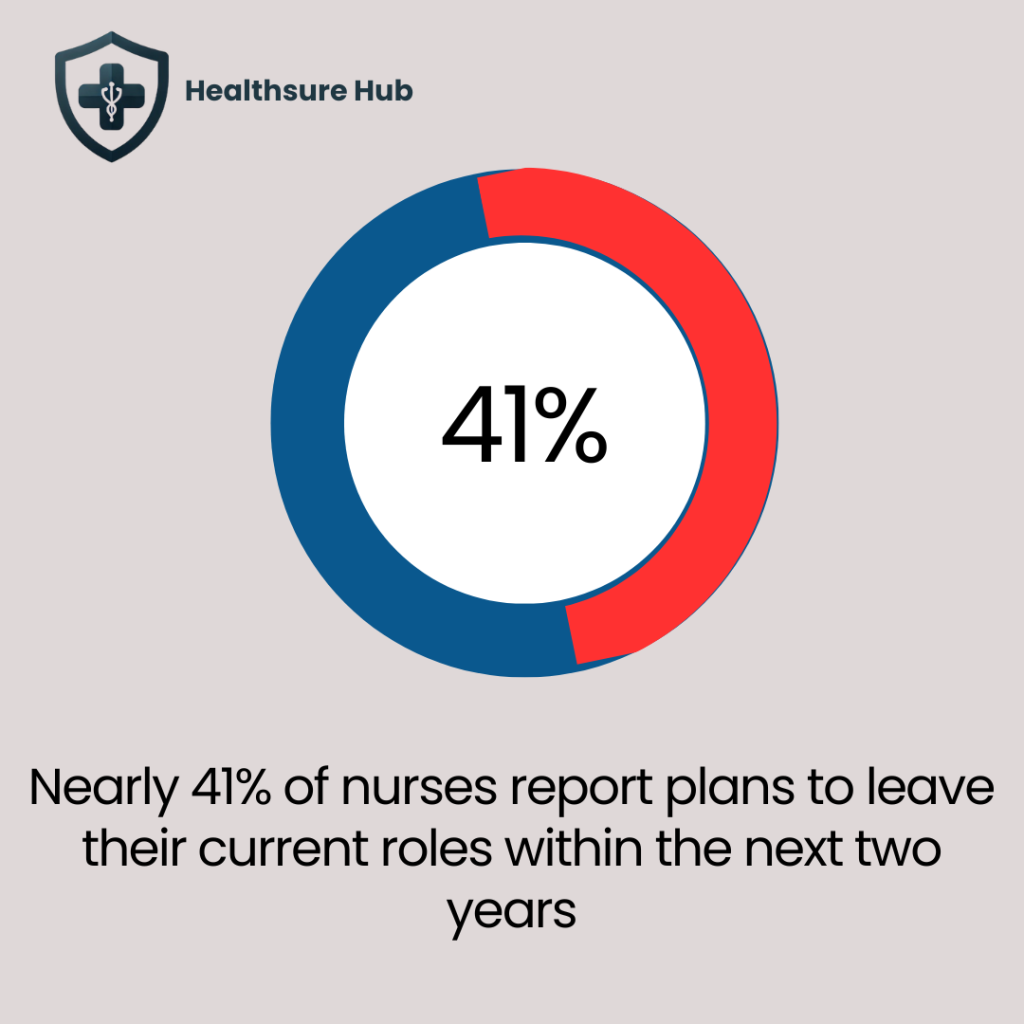
- Nearly 41% of nurses report plans to leave their jobs within two years, signaling continued workforce instability.
- More than 124,000 physician roles may remain unfilled by 2033, especially in primary care and specialty services.
- Burnout affects nearly half of physicians and over two-thirds of nurses, directly increasing turnover, absenteeism, and early retirement rates.
- Healthcare facilities with persistent staffing shortages experience higher hospital readmission rates, longer lengths of stay, and increased adverse events.
Why Healthcare Staffing Shortage Statistics Matter More Than Ever
Healthcare staffing shortage statistics matter because workforce availability directly determines care quality, patient safety, and system resilience. Staffing shortages are no longer isolated to rural regions or specific specialties. Instead, they reflect a structural imbalance between healthcare demand, workforce aging, and training capacity.
Hospitals experiencing chronic understaffing consistently report:
- Higher hospital readmission rates
- Increased emergency department congestion
- Longer patient wait times
- Reduced continuity of care
These outcomes make staffing data essential not only for administrators but also for policymakers, clinicians, and patients.
Healthcare Staffing Shortage Statistics and Trends
Understaffing in healthcare may come faster than what we expect. It’s happening as we speak. According to HRSA Health Workforce by 2037, the healthcare staffing shortage is expected to be of up to 187,130 full-time physicians, with more than 124,000 physician roles potentially remaining unfilled as early as 2033. This only signals the need for state and system-level capacity planning as soon as possible.
These shortages are closely tied to the aging physician workforce. A significant portion of practicing physicians are approaching retirement age, while training pathways remain lengthy and capacity constrained. At the same time, population growth and increasing chronic disease prevalence continue to expand demand for both primary and specialty care services.
Nursing Workforce Growth Masks Imminent Retirement Risk
Nursing staffing shortage statistics reveal a more complex picture. While the number of licensed registered nurses reached approximately 5.86 million in 2025, this growth masks a significant retirement-driven risk. An estimated one million nurses are expected to retire between 2027 and 2030, removing a substantial portion of experienced clinical staff from the workforce.
Experienced nurses are critical for patient monitoring, care coordination, and mentoring newer clinicians. As retirements accelerate, healthcare organizations face increased onboarding demands and potential skill gaps that can affect care consistency.
Importantly, licensure growth does not guarantee active bedside participation. Many licensed nurses work part time, transition into non-clinical roles, or leave acute care environments due to workload strain. These dynamics explain why staffing shortages persist despite rising license numbers. This year, the U.S. faces a shortage of over 500,000 RNs. With strict regulations and limited nursing schools this forces executives to prioritize retention alongside direct hire strategies just to maintain baseline coverage.
Behavioral Health Staffing Shortages
According to HRSA Health Workforce by 2037 the U.S. is expected to experience shortage of:
- 113,930 addiction counselors
- 87,840 mental health counselors
- 79,160 psychologists
- 50,440 psychiatrists
- 34,170 marriage and family therapists
- 39,710 school counselors
Rising Healthcare Labor Costs Reflect Staffing Shortages
The average registered nurse salary of $94,480 in 2025 highlights growing financial investment in healthcare labor. Competitive compensation plays an important role in attracting clinicians, particularly in regions facing severe shortages.
However, healthcare staffing shortage statistics consistently show that compensation alone does not resolve workforce challenges. Burnout, workload balance, professional autonomy, and organizational support remain equally influential in retention decisions. When higher pay is paired with supportive practice environments, staffing stability improves more sustainably.
Burnout Accelerates Attrition Across Clinical Roles
Burnout remains one of the most influential drivers within nursing staffing shortage statistics. Nearly half of physicians and more than two-thirds of nurses report experiencing burnout, which directly increases absenteeism, turnover, and early retirement.
Burnout reduces clinical engagement and contributes to workforce exits even among highly compensated professionals. Over time, this creates a self-reinforcing cycle where staffing shortages increase workload, which in turn accelerates burnout.
Healthcare systems that invest in workflow efficiency, mental health support, and staffing balance consistently report lower burnout rates and stronger retention.
Projected Shortages in the U.S. Mental Health Workforce
Healthcare staffing shortages statistics increasingly emphasize workforce instability rather than absolute headcount. Nearly 41% of nurses report plans to leave their current roles within the next two years, reflecting sustained pressure from workload intensity, scheduling challenges, and burnout.
High intent-to-leave rates contribute to frequent staff turnover, which disrupts team continuity and increases training and recruitment costs. Facilities experiencing rapid turnover often rely more heavily on temporary staffing, further increasing operational complexity.
Encouragingly, research shows that organizations prioritizing retention through supportive leadership, flexible scheduling, and manageable staffing ratios achieve greater workforce stability and improved care outcomes.
Staffing Shortages Directly Affect Patient Outcomes and Readmissions
Healthcare provider shortage statistics are closely linked to patient safety and hospital performance metrics. Facilities experiencing persistent staffing shortages report higher hospital readmission rates, longer lengths of stay, and increased adverse events.
Adequate staffing enables consistent patient monitoring, effective discharge planning, and timely follow-up care. When staffing levels are insufficient, care transitions become fragmented, increasing the likelihood of preventable complications and readmissions.
Improving staffing stability has been shown to strengthen care continuity, reduce avoidable utilization, and support better long-term outcomes for patients and providers alike.
What Healthcare Staffing Shortage Statistics Suggest Moving Forward
When examined together, healthcare staffing shortage trends highlight both ongoing challenges and clear opportunities. Workforce shortages are driven by predictable demographic trends, retention pressures, and demand growth rather than a lack of interest in healthcare careers.
Data consistently shows that healthcare systems focusing on retention, workforce planning, and supportive practice environments achieve more stable staffing levels and better patient outcomes. As these strategies scale, staffing shortages become more manageable and less disruptive to care delivery.
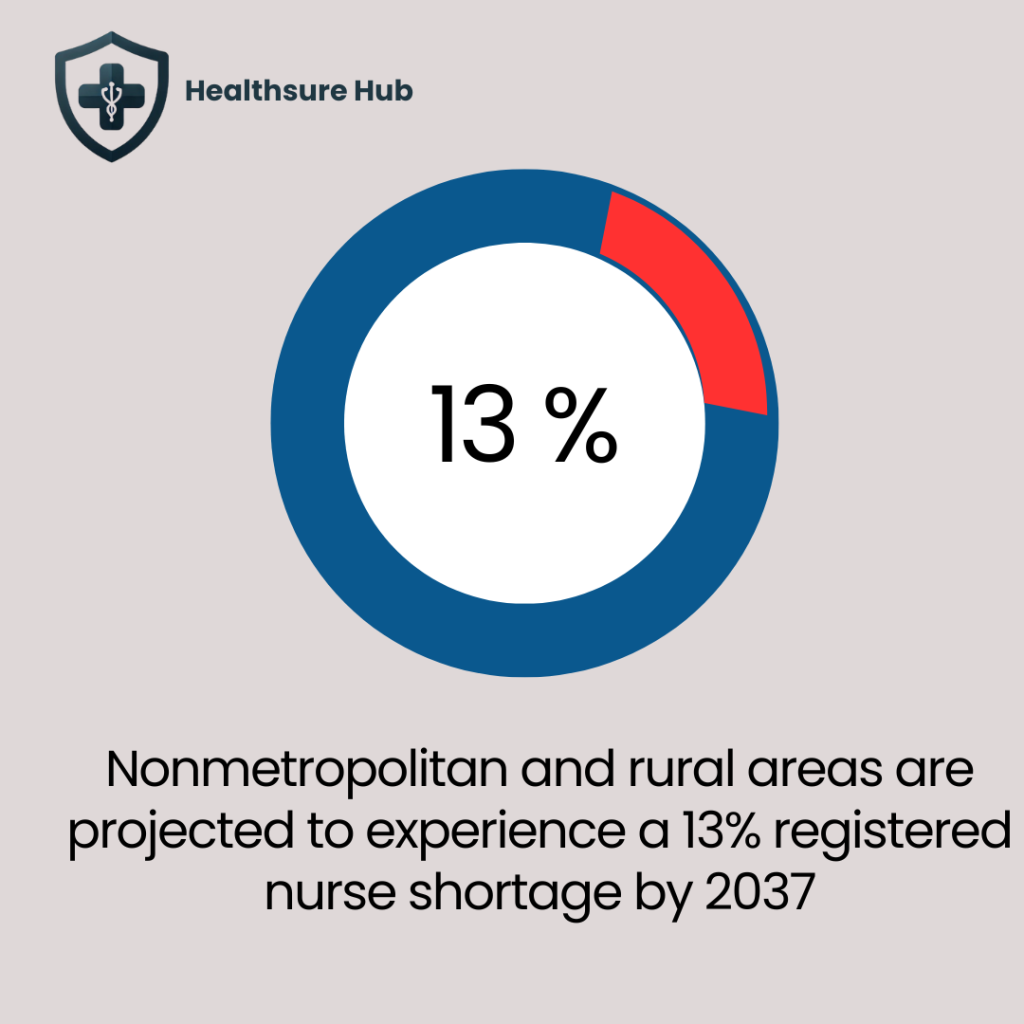
Rural and Nonmetropolitan Nursing Shortages Are Deepening
Healthcare staffing shortage statistics show that workforce gaps are not evenly distributed across the country. Nonmetropolitan and rural areas are projected to experience a 13% registered nurse shortage by 2037, significantly higher than shortages expected in many urban markets.
This disparity reflects long-standing challenges in rural healthcare delivery, including limited access to nursing education programs, fewer specialty practice opportunities, lower wage growth, and increased workload intensity. Rural hospitals and critical access facilities often operate with thinner staffing margins, making even small workforce losses operationally disruptive.
A 13% RN shortage in nonmetropolitan regions translates directly into reduced service availability, longer patient travel distances, and delayed care. These facilities also face greater difficulty replacing retiring nurses, as younger clinicians tend to cluster in metropolitan areas with broader career mobility and support infrastructure.
Conclusion
Healthcare staffing shortage statistics make one reality unmistakably clear: workforce capacity is now one of the most decisive factors shaping healthcare quality, access, and sustainability in the United States. Across physicians, nurses, and behavioral health professionals, the data consistently shows that shortages are not isolated events but interconnected trends driven by retirements, burnout, and rising patient demand.
Understanding these numbers is not only about anticipating gaps; it is about using data to strengthen continuity of care, reduce hospital readmissions, and ensure that healthcare systems are prepared to meet the needs of patients in the years ahead.
Sources:
https://www.aha.org/fact-sheets/2021-05-26-fact-sheet-strengthening-health-care-workforce
https://www.aacnnursing.org/news-data/fact-sheets/nursing-shortage
https://www.ncsbn.org/NND/Statistics/Aggregate-RNActiveLicensesTable.pdf
https://bhw.hrsa.gov/data-research/projecting-health-workforce-supply-demand
https://www.protouchstaffing.com/registered-nurse-salary-in-2025-how-much-do-rns-make
https://www.crosscountry.com/beyondthebedside
https://www.dewv.edu/impact-of-nursing-shortage-on-careers-2025-challenges-and-solutions/