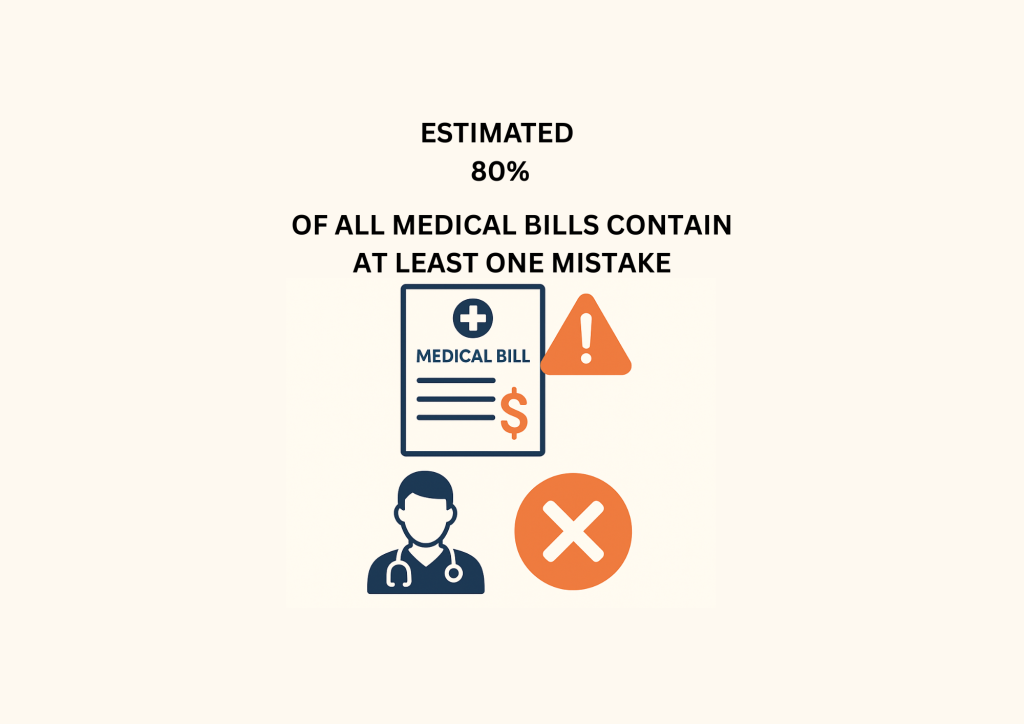
Imagine opening your medical bill only to find charges you don’t recognize, or worse, a bill that insurance should’ve fully covered. You’re not alone. Medical billing errors are so widespread that nearly 8 out of 10 of U.S. medical bills contain at least one mistake. The errors present in the bills could cost you thousands, delay the needed care, even destroy the trust in the U.S. medical system.
The hidden costs extend far beyond your wallet. From denied claims to surprise bills, medical billing errors statistics reveal a healthcare system struggling with inefficiencies that affect millions of Americans every year.
Healthsure Hub breaks down the top 10 shocking medical billing errors statistics you need to know in 2025, and explore how these errors impact patients, providers, and the broader healthcare industry.
Top 10 Medical Billing Errors Statistics
- 49-80% of medical bills contain at least one error.
- U.S. physicians lose an estimated $125 billion each year due to billing mistakes.
- Hospitals lose an estimated $68 billion annually from billing mistakes.
- 10% or more of claims are denied for a growing number of providers.
- 36% of US households had medical debt in 2024.
- 86% of denials are potentially avoidable.
- 15 million Americans have medical bills on their credit reports due to billing mistakes.
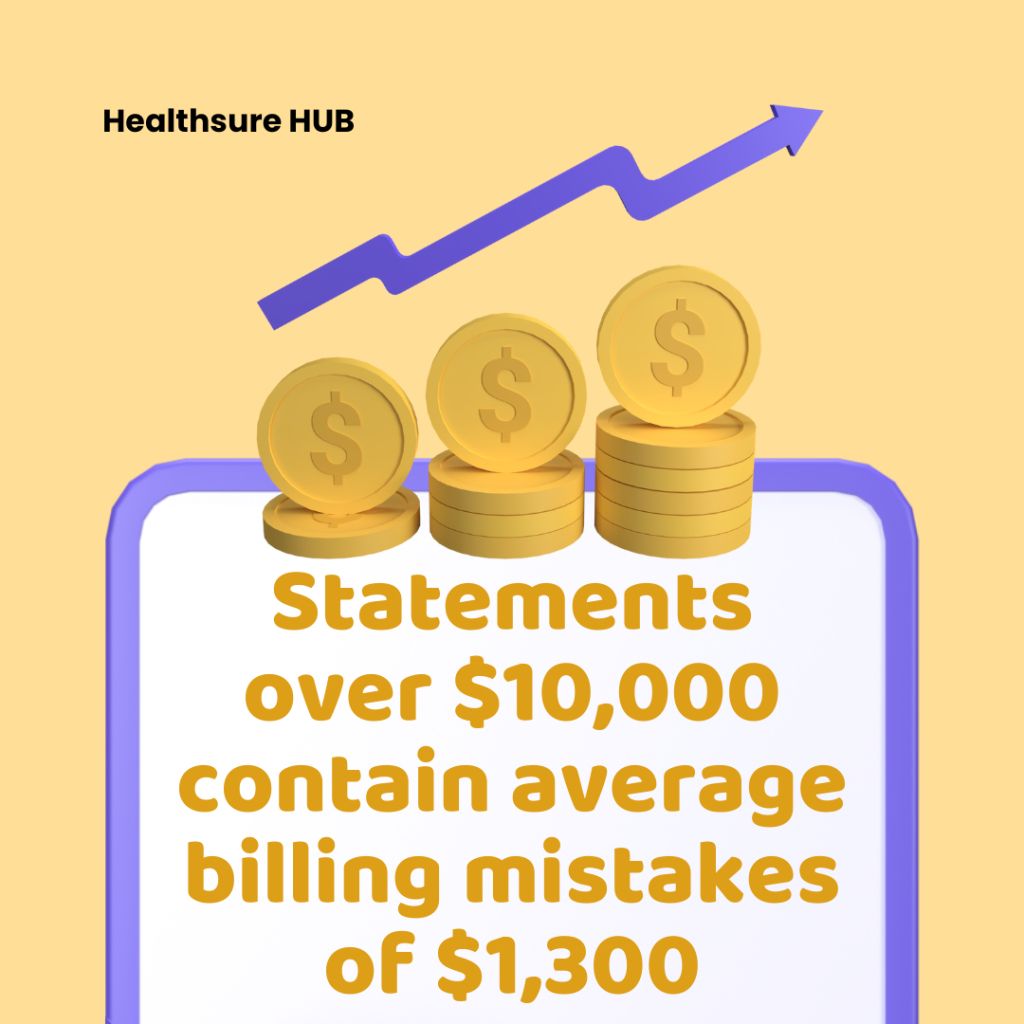
- Bills over $10,000 contain an average billing error of $1,300.
- Over 45% of insured adults received a bill for a service they believed insurance should cover.
- Insurers reject 1 in 7 claims across private plans, yet only 0.1% of denied ACA claims are appealed.
Medical Billing Errors Statistics Overview
An estimated 80% of all medical bills contain at least one mistake, making billing inaccuracies one of the most consistently documented pain points in the industry. Such a high error rate affects individuals across all demographics starting from insured and uninsured patients to seniors on Medicare. Such high billing error rates create more than just minor inconveniences; they pose a significant repercussions for:
- Patients
- Provides
- Healthcare practices
The range of 49-80% of medical bills containing at least one mistake is based on studies from healthcare researchers. While their research reflects other methodologies, one thing that remains certain is that errors in medical bills are far more common than we might think.
Large-scale reports consistently show that millions of Americans experience incorrect codes, duplicate charges, mismatched patient information, or inflated pricing. These statistics emphasize the scale of the problem: from routine physician visits to major surgeries, billing inaccuracies have become a common part of the healthcare experience. With such a large portion of healthcare transactions affected, patients may start doubting the U.S. healthcare system and the reliability of the medical staff.
U.S. Medical Billing Errors Statistics
Across the United States, medical billing errors statistics highlight how deeply embedded inaccuracies are in the healthcare system. The data shows that billing mistakes appear in claims of every size, from routine doctor visits to major surgeries. A significant portion of billing discrepancies appear in high-value claims, especially those exceeding $10,000, where the average error reaches $1,300 per bill.
Physician and Hospital Billing Loss Statistics
Financial losses linked to billing errors are staggering. Medical billing errors statistics show that U.S. physicians lose an estimated $125 billion each year, or about $5 million per provider. This occurs due to inaccurate coding, claim errors, and administrative inefficiencies. The losses directly affect revenue cycles, staffing demands, and the long-term sustainability of smaller practices.
Hospitals face equally substantial financial consequences. In 2022, the hospitals around the U.S. lost a projected $68 billion annually due to:
- Billing mistakes
- Wrong codes
- Rejected claims
- Lost payments from in-house systems
Together, these physician and hospital loss statistics underscore the heavy economic toll that billing inaccuracies impose on healthcare providers nationwide. The solution to the problem might be outsourcing the entire billing function. By 2033, it’s believed that the U.S. medical billing outsourcing market will hit $46.17 billion, offering a chance for a better and regulated healthcare system.
Medical Claim Denial Statistics
Claim denials continue to be one of the strongest indicators of medical billing accuracy. A growing number of providers experience 10% or more of their claims being denied, contributing to significant operational challenges. Even more striking is that 86% of claim denials are potentially avoidable, meaning the majority stem from correctable issues such as data entry errors or missing information.
Insurance rejection trends remain significant as well. Private insurers reject 1 in 7 claims, and yet only 0.1% of denied ACA marketplace claims are appealed. This gap highlights how millions of denied claims go unchallenged each year, despite the high percentage of preventable errors noted in medical billing errors statistics.

Medical Debt Statistics and Billing Error Impacts
Medical debt remains a defining issue in the U.S., and billing errors play a measurable role. According to medical debt statistics, in 2024, 36% of U.S. households carried medical debt, affecting families across all income levels. Incorrect or inflated billing can significantly increase the amount patients owe, particularly for high-cost treatments or ongoing care.
Medical billing errors statistics also show that debt linked to inaccuracies frequently becomes long-term. Many individuals receive surprise bills, unclear statements, or charges they assumed were covered by insurance; issues that can compound quickly when not resolved early. As household medical debt continues to rise, billing mistakes remain a significant contributor to the country’s broader financial burden.
Medical Billing Errors Statistics in Credit Reporting
Billing errors also have lasting implications on personal credit. Approximately 15 million Americans currently have medical bills on their credit reports that stem from billing mistakes, insurance miscommunication, or unresolved disputes. These inaccuracies often appear when a bill is sent to collections before the patient has an opportunity to review or correct the charges.
Because medical credit issues can lower scores, affect loan eligibility, and create long-term financial strain, the scale of these inaccuracies shows how deeply medical billing errors statistics overlap with broader financial protection concerns. For many consumers, a single billing error can have lasting consequences long after the medical visit has ended.
High-Cost Billing Error Statistics
Large medical bills carry the highest likelihood of errors. Statements over $10,000 contain average billing mistakes of $1,300, demonstrating how the complexity of high-cost care often leads to greater inaccuracies. These discrepancies may include duplicate charges, incorrect coding, or misapplied insurance adjustments.
Medical billing errors statistics show that these high-dollar mistakes create substantial financial disruption for both patients and providers. For patients, they can dramatically inflate out-of-pocket costs. For providers, they contribute to increased disputes, slower reimbursement, and more intensive administrative review processes.
Insurance Coverage Discrepancy Statistics
A growing body of medical billing error statistics reveals that billing issues frequently intersect with insurance misunderstandings. More than 45% of insured adults received a bill for a service they believed insurance should have covered, suggesting a significant gap between expected coverage and how claims are ultimately processed.
These discrepancies often arise from inconsistent coding, mismatched documentation, or differences between provider and insurer interpretations. Regardless of the source, the statistics show that insured individuals routinely face billing surprises that contribute to medical debt, credit issues, and broader financial stress.
Insurance Rejection and Appeals Statistics
Medical billing errors statistics show that insurers deny claims at notable rates, but appeals almost never happen. Private insurers reject 1 in 7 claims, reflecting a substantial portion of the healthcare billing pipeline. Despite this, only 0.1% of denied ACA marketplace claims are appealed, meaning the overwhelming majority of rejected claims go unchallenged.
Given that 86% of denials are considered potentially avoidable, the low appeal rate contributes to billions in lost payments and inflated patient balances. These statistics highlight an ongoing gap between denied claims and the actions taken to correct them, reinforcing the importance of accurate initial billing and effective follow-up.
Conclusion
Medical billing errors statistics make one thing clear: inaccuracies are widespread, costly, and deeply felt across the U.S. healthcare system. With up to 80% of bills containing mistakes, rising medical debt, and millions affected by avoidable denials or credit report issues, these errors continue to impact both patients and providers every day.
The data underscores a simple truth –-greater accuracy, transparency, and awareness remain key to reducing the financial strain caused by medical billing mistakes.
Sources:
https://orbdoc.com/blog/medical-bill-errors-80-percent-problem
https://coniferhealth.com/wp-content/uploads/31928faf-b605-4bf9-9049-a5c8f4575310_CRI_Insert.pdf
https://humanmedicalbilling.com/blog/68-billion-lost-why-in-house-billing-must-go
https://pmc.ncbi.nlm.nih.gov/articles/PMC12394938
https://abcnews.go.com/GMA/story?id=127077&page=1