Every year, healthcare providers unknowingly receive millions of dollars in excess payments, funds they are legally obligated to return. Unlike denied claims or underpayments, overpayments in medical billing often go unnoticed, silently skewing financial reports and exposing practices to audits, fines, and reputational risk. Yet, many organizations fail to recognize that overpayments aren’t just accounting errors, but compliance liabilities that can carry serious legal consequences.
This article breaks down what overpayment in medical billing really is, why it matters, how it happens, and the proven strategies healthcare providers can use to manage, recover, and prevent it, protecting both their revenue and their credibility.
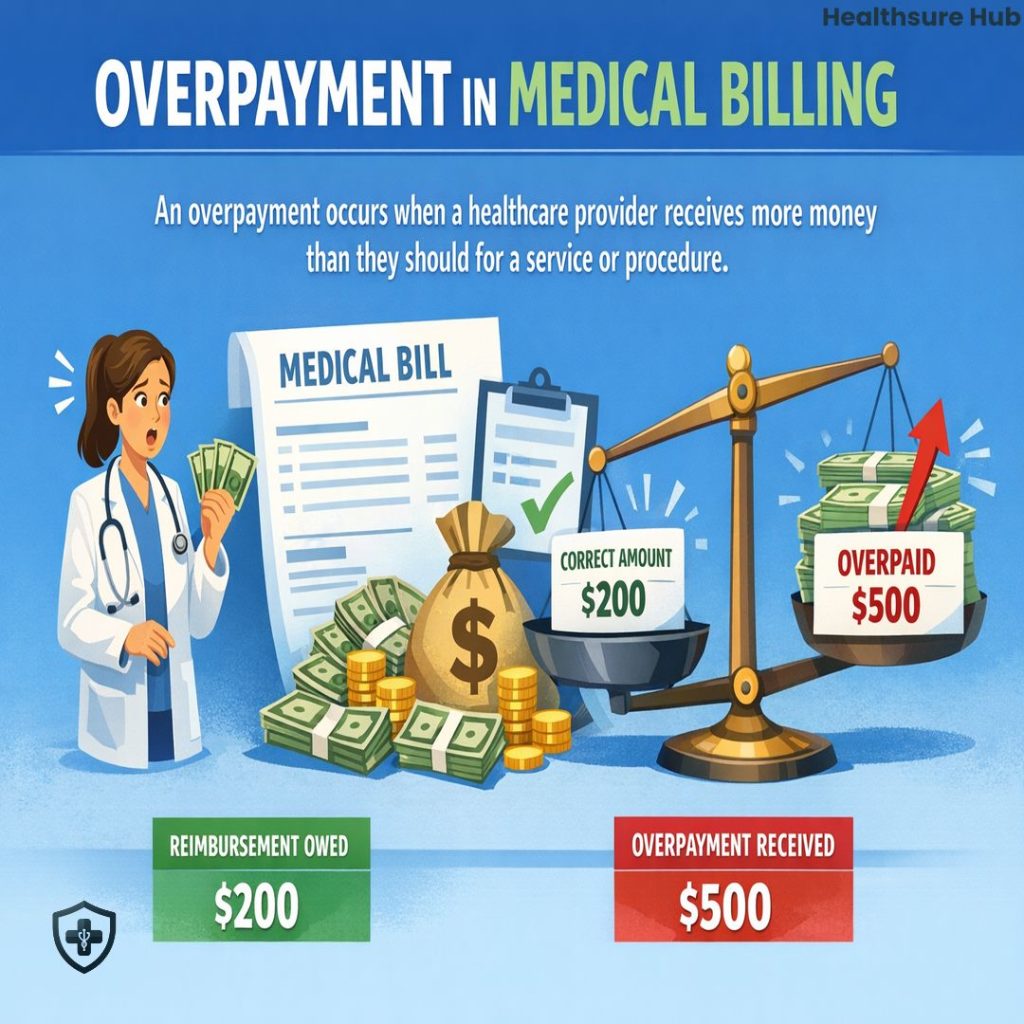
What Is an Overpayment in Medical Billing?
Overpayment in medical billing occurs when a healthcare provider receives more money than they should’ve for a service, procedure, or encounter than what they’re owed according to their reimbursement rate. The excess payment may come from a patient, a commercial insurance payer, or a government program such as Medicare or Medicaid.
From a compliance perspective, an overpayment is not income. It is a liability. Once identified, it represents a debt that must be returned or adjusted within required timeframes. Overpayment can result from provider errors, payer errors, or patient payment discrepancies, but the obligation to address it ultimately rests with the provider.
Importantly, overpayment in medical billing is defined by entitlement, not intent. Whether the excess payment occurred accidentally or due to a system error is irrelevant. What matters is that the provider received more than allowed under the applicable fee schedule, contract, or benefit plan. Common causes of overpayments are:
- Incorrect or duplicate billing codes
- Lack of communication between providers and payers
- Use of outdated billing software
- Patients paying more because of unregulated cost estimates and insurance misunderstandings
Why Overpayment Is Important in Medical Billing
Overpayment in medical billing is important because it sits at the intersection of compliance, financial integrity, and trust. When overpayments are mishandled, the consequences extend far beyond a single refund.
Legal Risk
From a regulatory standpoint, providers are required to monitor payments and return identified overpayments within established deadlines. Failure to do so can trigger enforcement actions, civil penalties, and allegations under federal and state laws. Overpayment in medical billing is closely scrutinized during audits because it signals weaknesses in internal controls and billing accuracy.
Financial Problems
Financially, overpayments distort revenue reporting. Retaining funds that should not be recognized as income creates inaccurate financial statements, complicates reconciliations, and increases exposure during payer or government audits. Over time, unresolved overpayment in medical billing can undermine the reliability of a practice’s revenue data.
Lack of Trust Between Providers and Patients
Equally important is trust. Patients expect transparency when they are charged for care. Payers expect contractual compliance. When overpayment in medical billing is discovered by someone other than the provider, whether a patient or an insurer, it raises questions about integrity and accountability.
Overpayment vs Underpayment in Medical Billing
Although both affect cash flow, overpayment and underpayment in medical billing are fundamentally different problems and must be managed separately.
Underpayment occurs when a provider is reimbursed less than the allowed amount and must pursue additional payment. Overpayment in medical billing occurs when reimbursement exceeds what is permitted and requires correction or return. Underpayments represent lost revenue opportunities; overpayments represent compliance liabilities.
Confusion between the two often arises during payment posting and reconciliation. A clean revenue cycle process tracks both conditions independently, making sure that overpayment is identified quickly while underpayments are pursued through appeals or follow-up.
Common Causes of Overpayment
Overpayment rarely stems from a single failure. It is usually the result of breakdowns across systems, workflows, and communication.
Provider-related causes are among the most common. Coding errors, incorrect modifiers, duplicate claim submissions, and inaccurate charge entry can all lead to overpayment. Inadequate insurance verification before services are rendered also increases the likelihood of patient overpayments.
Payer-related causes are equally significant. Insurance companies may process claims incorrectly, apply the wrong reimbursement rate, or issue duplicate payments. Coordination of benefits errors, especially when multiple payers are involved, frequently result in overpayment in medical billing even when claims are submitted correctly.
Patient-related causes typically occur when payments are collected before insurance adjudication. Copays, deductibles, and coinsurance amounts may change after a claim is processed, leaving an excess balance on the patient’s account. Without careful reconciliation, these amounts become patient overpayments.
How Insurance Companies Identify and Recover Overpayments
Insurance companies actively monitor claims for overpayment in medical billing. This process is far more systematic than many providers realize.
Payers use automated payment integrity systems, retrospective claim reviews, and targeted audits to identify payments that exceed contractual or benefit limits. When overpayment is detected, payers typically recover funds in one of two ways.
The first method is an offset. Instead of requesting a refund, the payer reduces future reimbursements until the overpaid amount is recovered. These adjustments appear on remittance advice and can easily be missed if payment posting is not reviewed carefully.
The second method is a refund request or recoupment notice. In this case, the payer formally notifies the provider of the overpayment and requests repayment within a specified timeframe. Failure to respond may result in escalation, interest charges, or broader audits.
Understanding how payers recover overpayment helps providers anticipate adjustments and maintain accurate accounts receivable records.
Legal and Compliance Requirements for Overpayments
Overpayment in medical billing carries explicit legal obligations, particularly for Medicare and Medicaid providers. Federal law requires providers to report and return identified overpayments within established deadlines, commonly referred to as the “60-day rule.”
The countdown begins when an overpayment is identified, not when the final dollar amount is calculated. Recent regulatory updates allow providers a limited suspension period to conduct a good-faith investigation when determining whether an overpayment is isolated or part of a broader issue. This flexibility does not eliminate the obligation to act promptly.
Under the CMS 60-day rule healthcare providers are required to:
- Identify payments via internal audits
- Determine the exact amount that’s been overpaid within the timeframe
- Refund overpayment within 60 day of identification
- Keep records to show you’re in compliance with the rule
Failure to return overpayment can expose providers to liability under civil enforcement statutes, and could result in violations of the False Claims Act. Failure to return the overpayment within the set timeframe could result in hefty fines of up to $11,000 fine per claim. Worst case scenario, healthcare provides could be excluded from Medicare and Medicaid programs. In some cases it could go as far as the provider being criminally prosecuted.
Compliance requires documentation, transparency, and timely action. Overpayment must be treated as a regulatory issue, not a routine accounting adjustment.

How to Handle Patient Overpayments
Patient overpayment requires a careful balance of accuracy and communication. Key steps for handling patient overpayments are:
- Identify the overpayment– The first step is identification through routine account reconciliation and review of explanation of benefits.
- Notify the patient – The patient should be notified promptly and clearly. Transparency matters. Patients should understand why the overpayment occurred and how it will be resolved. Providers could contact the patient via phone call, email or formal letter explaining the situation of why and how the overpayment occurred.
- Offer refunds – Provides can offer a prompt refund or applying a credit to future services may be appropriate. In others, a direct refund is necessary.
- Document everything – Regardless of the method, documentation is essential. Every patient overpayment in medical billing should be supported by records showing identification, communication, and resolution.
How to Handle Insurance Overpayments
Insurance overpayment is more procedural but no less important. Verification is critical. Healthcare provides need to:
- Verify the overpayment – Providers should review remittance advice, contracts, and claim details to confirm that an overpayment occurred.
- Contact the payer – Once verified, providers should reach out to the insurance’s billing department to clarify discrepancies. Open communication is the ultimate goal here.
- Process the refund – Providers should follow payer-specific instructions for refunds or adjustments. Some payers prefer offsets, while others require direct repayment.
- Document everything – Clear documentation protects the provider if questions arise later.
Consistent handling of insurance overpayment in medical billing reduces audit risk and demonstrates good-faith compliance.
How to Prevent Overpayment
Preventing overpayment in medical billing begins with accurate front-end processes. Insurance verification, eligibility confirmation, and clear patient financial communication reduce errors before claims are submitted.
On the back end, updated billing systems, regular internal audits, and well-trained staff play a critical role. Payment posting should include routine checks for duplicate payments and unexpected reimbursement amounts.
Clear internal policies ensure that overpayment is identified, documented, and resolved consistently across the organization. To prevent overpayment healthcare providers could:
- Invest in a new, updated billing software
- Use correct coding standards
- Provide staff training
- Verify patient coverage at intake
- Outsource medical billing services if necessary
Conclusion
Overpayment in medical billing is not a minor inconvenience or an accounting footnote. It is a compliance obligation, a financial accuracy issue, and a measure of operational maturity. Practices that understand overpayments, monitor payments proactively, and act decisively when excess funds are identified protect themselves from risk while strengthening trust with patients and payers.
A proactive approach to overpayment transforms a common vulnerability into a demonstration of accountability and professionalism, qualities that define sustainable, compliant healthcare organizations.