Medical billing may seem simple at first glance: submit a claim, receive a payment, and move on. But behind the scenes, the process is far more complex, involving multiple steps that make your practice get paid accurately and promptly. One of the most critical steps in this process is payment posting in medical billing.
Our team at Healthsure Hub explains what payment posting is in medical billing, how it works, and why it matters is essential for healthcare providers, billing staff, and practice managers alike. Accurate payment posting ensures proper cash flow, reduces errors, and strengthens patient trust.
What is Payment Posting in Medical Billing?
At its core, payment posting in medical billing is the process of recording payments, adjustments, and denials from insurance companies and patients directly into your billing system. It’s a careful process that ensures every payment received aligns with the corresponding claim, guaranteeing accuracy and transparency in your practice’s financial records. Without it, patients can experience confusion about their financial obligations while practices experience significant reimbursement lags.
Think of it like balancing a checkbook, but for an entire medical practice. Every payment, whether from a patient’s co-pay, deductible, or an insurance reimbursement, needs to be accounted for, applied to the correct account, and reconciled with bank deposits.
Why Payment Posting in Medical Billing Matters
You might think that once you send a medical bill, that’s it, there’s nothing else to do. This is where you’re wrong. Payment posting is the backbone for your healthcare practice to run smoothly without interruptions.
Without accurate payment posting in medical billing, a practice’s financial records can experience a host of issues such as:
- Revenue leakage – unposted or misposted payments can lead to lost revenue.
- Claim denials – errors in posting can create discrepancies, prompting unnecessary claim denials.
- Patient dissatisfaction – incorrect balances confuse patients and can damage trust.
Inefficient workflows – billing staff spend extra time correcting errors, reducing productivity.
More than that, accurate payment posting helps providers to easily identify trends and issues with their payments. Through careful analysis, healthcare practices can spot frequent denials or underpayments from certain issues. By ensuring accurate payment posting, practices can maintain financial health, streamline operations, and provide patients with transparent billing.
Payment posting is important for reducing errors and discrepancies. With $68 billions being lost to medical billing errors, payment posting prevents financial losses and reduces time in fixing billing mistakes.
Types of Payment Posting in Medical Billing
Payment posting in medical billing can be performed manually or through automated systems, each with its own benefits and drawbacks.
Manual Payment Posting
In manual posting, billing staff enter payment details from EOBs or ERAs into the billing system. This method allows for human oversight and verification but is time-consuming and prone to errors, especially in high-volume practices. Manual payment posting is better for smaller practices or when automated payment posting is not available.
Challenges of manual posting
- Higher likelihood of data entry errors
- Slower processing times
- Greater risk of missed payments or misapplied amounts
Automated Payment Posting
Automated payment posting uses software to import and reconcile payments directly from electronic remittance advice (ERA) or EOBs. Many modern EHRs and billing platforms can automatically apply payments to the correct patient accounts, flag discrepancies, and update records in real-time, making it perfect for larger companies that deal with a great deal volume of transactions.
Benefits of automation
- Faster, more efficient posting
- Reduced human error
- Immediate reconciliation with bank deposits
- Easier tracking of denials and adjustments
Most large or growing practices benefit from automation, while smaller practices may still rely on a hybrid approach combining manual and electronic posting.
Key Documents in Payment Posting
To post payments accurately, billing teams rely on key documents that provide essential payment details:
Explanation of Benefits (EOB)
Explanation of Benefits (EOB) is a statement from an insurance company that details what services were billed, how much was covered, the amount the insurer paid, and the patient’s remaining responsibility. EOBs are usually claim-specific and serve as a primary reference for payment posting.
Electronic Remittance Advice (ERA)
Electronic Remittance Advice (ERA) are electronic files provided by insurers that summarize multiple claim payments at once. They allow for faster processing, automated reconciliation, and easier tracking of adjustments or denials across multiple claims.
Electronic Fund Transfers (EFTs)
Electronic Fund Transfers (EFT) represent the actual transfer of funds from the payer to the provider. While ERAs and EOBs show the details, EFTs confirm that payments have been deposited into the practice’s bank account.
Accurate payment posting in medical billing involves carefully cross-referencing all three: the EOB or ERA outlines what should be paid, and the EFT confirms what was actually received.

Step-by-Step Payment Posting Workflow
Accurate payment posting in medical billing follows a series of precise steps that ensure no payment is overlooked and all records are reconciled.
- Receiving Payment Information – payments arrive through multiple channels: checks, credit cards, and is accompanied by an Explanation of Benefits (EOBs) or Remittance Advice (RA). Each payment is categorized according to its source and type.
- Verifying Payment Details – the billing team reviews payment information, comparing it with the corresponding claim. This step ensures the amount received matches the billed amount.
- Posting Payments – payments are being recorded in the billing system and applied to the correct patient accounts. This step updates outstanding balances and ensures accurate financial reporting.
- Recording Adjustments and Write-offs – contractual allowances, co-pays, deductibles, and write-offs for non-covered services are applied. These adjustments prevent inflated balances and maintain compliance with payer agreements.
- Posting Secondary and Tertiary Insurance Payments – if a patient has multiple insurance plans, payment posting accounts for payments from primary, secondary, and even tertiary insurers, ensuring full reconciliation of all claims.
- Managing Denials and Rejections – any denied or partially paid claims are flagged for follow-up. Understanding why a claim was denied helps prevent future errors and ensures timely resubmission.
- Reconciliation with Bank Deposits – payments posted in the system are reconciled with bank statements or EFTs. This step guarantees that all funds are accounted for.
- Reporting and KPIs – finally, reporting tools track key performance indicators such as posting accuracy, turnaround time, and denial resolution rates. These metrics help optimize workflow and financial health.
Common Issues and Challenges in Payment Posting
Even with well-established processes, payment posting in medical billing can face a variety of issues and challenges that impact cash flow, accuracy, compliance, and overall practice efficiency. Understanding these risks is key to preventing revenue loss and maintaining accurate patient accounts.
- Misapplied Payments – payments applied to the wrong patient account or service are a frequent issue. Misapplied payments can lead to inaccurate balances, frustrated patients, and time-consuming corrections for billing staff.
- Duplicate Payments – posting the same payment twice can skew financial records, create confusion, and require additional reconciliation to correct errors.
- Denied or Underpaid Claims – payments that don’t match the expected amounts, or claims denied by insurers, can disrupt cash flow. Plenty of the denied claims are never submitted, meaning there’s a lot of money still lying on the table.
- Incorrect Adjustments or Write-offs – misapplied contractual allowances, co-payments, deductibles, or write-offs can distort financial records, complicate audits, and reduce revenue accuracy.
- Delayed Secondary Payments – for patients with multiple insurance plans, slow processing of secondary or tertiary payments can extend the revenue cycle, causing longer outstanding balances.
- Manual Processing Inefficiencies – manual entry of payment information is time-consuming and prone to human error, especially in high-volume practices. Errors can include misapplied payments, duplicate entries, or missed postings, all of which slow down reconciliation.
- Insufficient Knowledge or Training – payment posting in medical billing requires a solid understanding of EOBs, ERAs, payer rules, and adjustments. Staff without proper training may make mistakes that result in claim denials, delayed payments, or incorrect patient balances.
- Long Payment Cycles – slow payments from insurers or patients can create cash flow challenges. Without timely posting and reconciliation, revenue may be delayed, and accounts receivable can become difficult to manage.
- Compliance Adherence Challenges – Practices must stay in compliance with HIPAA and other regulatory standards when handling patient financial data. Improper posting, poor documentation, or mishandling of sensitive information can lead to audits or penalties.
- Fraud Exposure – handling sensitive financial information carries inherent risks. Without proper checks and monitoring, there’s potential for fraud, misappropriation of funds, or unauthorized adjustments.
Addressing these issues and challenges requires a combination of staff training, standardized processes, workflow automation, and regular audits. Implementing these measures ensures payment posting in medical billing is accurate, efficient, secure, and supportive of overall revenue cycle management.
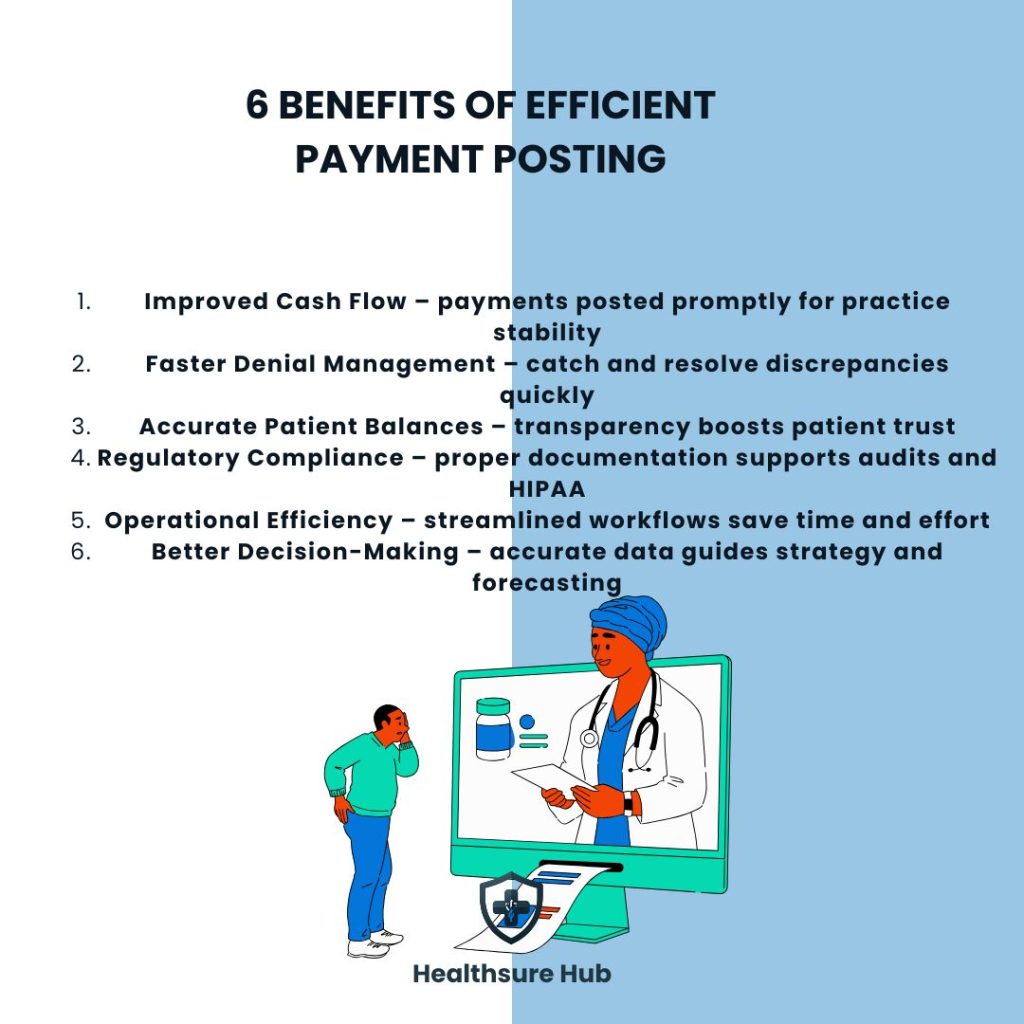
Benefits of Efficient Payment Posting
When done correctly, payment posting in medical billing provides multiple benefits:
- Improved Cash Flow – ensures all payments are posted promptly, supporting practice stability.
- Faster Denial Management – early identification of discrepancies allows for quicker resolution.
- Accurate Patient Balances – transparency improves patient satisfaction and trust.
- Regulatory Compliance – proper documentation aids in audits and HIPAA compliance.
- Operational Efficiency – streamlined workflows reduce administrative burden and save time.
- Better Decision-Making – accurate data informs revenue forecasting and strategic planning.
Tools and Technology to Improve Payment Posting
Modern tools can significantly improve the accuracy and speed of payment posting in medical billing:
- Automated ERA processing – import and apply multiple claim payments simultaneously.
- EHR/Billing system integration – streamlines workflow and prevents duplicate data entry.
- Clearinghouses – act as intermediaries between your practice and insurance companies, ensuring electronic claims and payments flow smoothly.
- Reporting dashboards – track payment trends, denial rates, and account balances for informed decision-making.
These tools allow practices to reduce manual effort, minimize errors, and accelerate revenue collection.
Conclusion
Understanding what is payment posting in medical billing and implementing a structured, accurate process is critical to the success of any healthcare practice. From ensuring cash flow and reducing billing errors to improving patient satisfaction and compliance, payment posting is a cornerstone of efficient revenue cycle management.
By following best practices, leveraging modern tools, and training your staff effectively, your practice can turn payment posting from a routine administrative task into a strategic advantage.