Medical billing is complex, and even minor errors can have major financial consequences. One of the most critical, yet often overlooked, aspects of billing is recoupment. Whether it’s a large hospital system or a small practice, recoupment can disrupt cash flow, increase administrative workload, and trigger compliance concerns.
Understanding recoupment in medical billing is not just about responding to a payer’s request, it’s about maintaining financial accuracy, safeguarding your revenue cycle, and preventing future losses. This article provides a clear, step-by-step guide on recoupment in medical billing: what it is, why it happens, how the process works, its impact on providers, and strategies to prevent and manage it effectively.
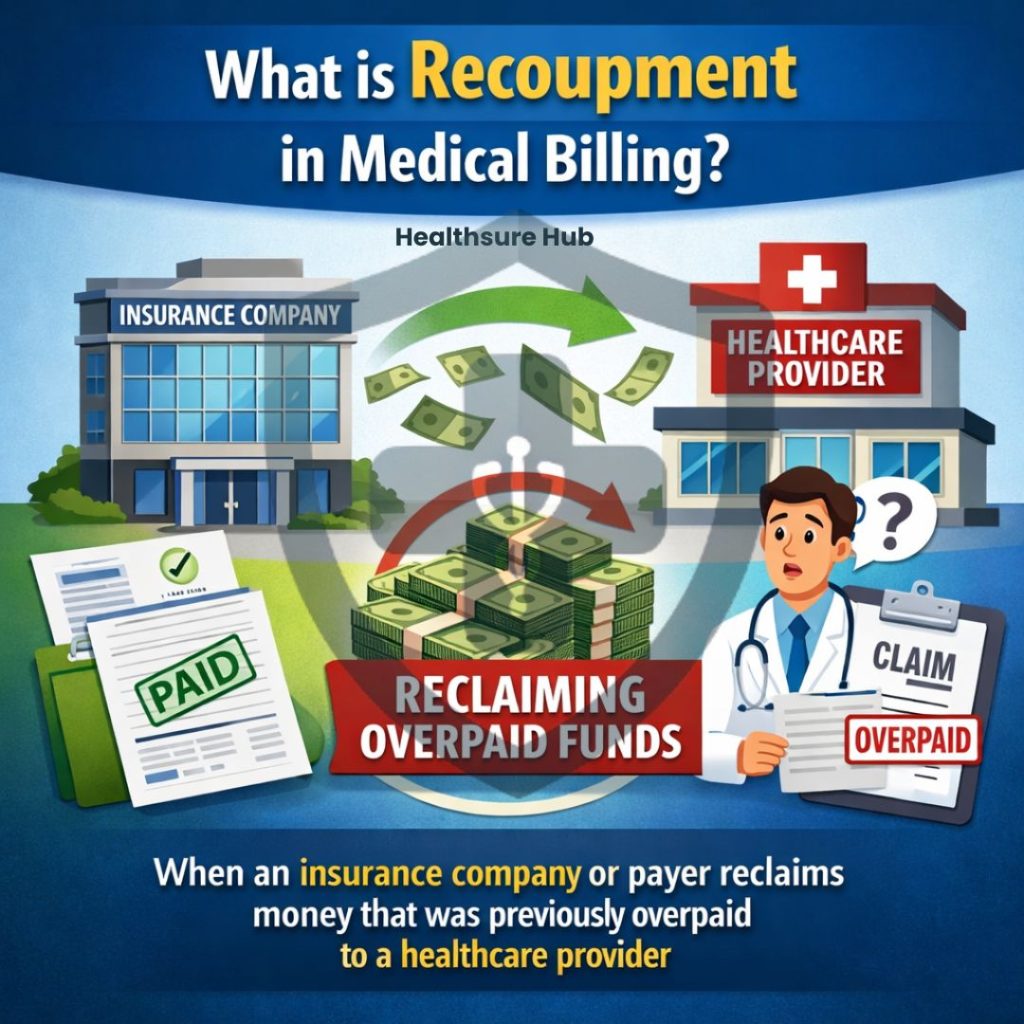
What is Recoupment in Medical Billing?
Recoupment occurs when an insurance company or payer reclaims money that was previously overpaid to a healthcare provider. Unlike claim denials, which prevent payment upfront, recoupment happens after payment has been made, making it a post-transaction correction.
Common triggers for recoupment include:
- Billing errors (duplicate claims, miscoding)
- Contractual adjustments (updates to reimbursement rates or coverage terms)
- Administrative errors (missing documentation, inaccurate patient information)
- Non-compliance with payer guidelines (incorrect use of codes, lack of pre-authorizations)
- System errors (automated miscalculations by payers)
At its core, recoupment ensures that payments reflect actual services rendered and that both providers and payers maintain compliance with contractual and regulatory standards.
Reasons for Recoupment in Medical Billing
Recoupment always stems from overpayments, situations where a provider is reimbursed more than the amount due for a service. Overpayments can arise from multiple sources:
- Billing Errors – with 80% medical billing errors containing at least one mistake such as duplicate claims or incorrectly coded services, it can inflate reimbursements. These errors often result from human oversight or complex coding rules.
- Administrative Mistakes – Simple data entry errors, missing documentation, or inaccurate patient details can trigger overpayments that later require recoupment. This is the same as when a simple error enters in the patient folder information that could result in a claim being processed incorrectly.
- Contractual Misalignment – Changes in reimbursement rates, bundled services, or contract terms may not be reflected immediately in billing systems, causing discrepancies.
- Coordination of Benefits (COB) Errors – When a patient has multiple insurance plans, payments may be incorrectly allocated, leading to overpayment by one payer.
- System or Process Errors – Less common, but automated payer systems can occasionally process claims incorrectly, generating overpayments.
By understanding these root causes, providers can implement controls that reduce the frequency and financial impact of recoupments.
Types of Recoupment in Medical Billing
Not all recoupments are the same. Understanding the specific type of recoupment in medical billing is essential for determining the appropriate response:
| Type | Description | Common Trigger |
| Audit-Based | Payer reclaims payments after reviewing claims and records | Coding errors, medical necessity issues |
| COB Recoupment | Recovery when multiple insurers are involved | Wrong primary payer billed |
| Duplicate Claim | Same claim paid twice | Resubmission errors, system glitches |
| Contractual Adjustment | Payment corrected based on contract terms | Misapplied rates, bundled services |
| Government Payer | CMS, Medicare, or Medicaid recoup overpayments per federal guidelines | Compliance reviews, audits |
Knowing the type helps providers prepare evidence, respond strategically, and minimize financial impact.
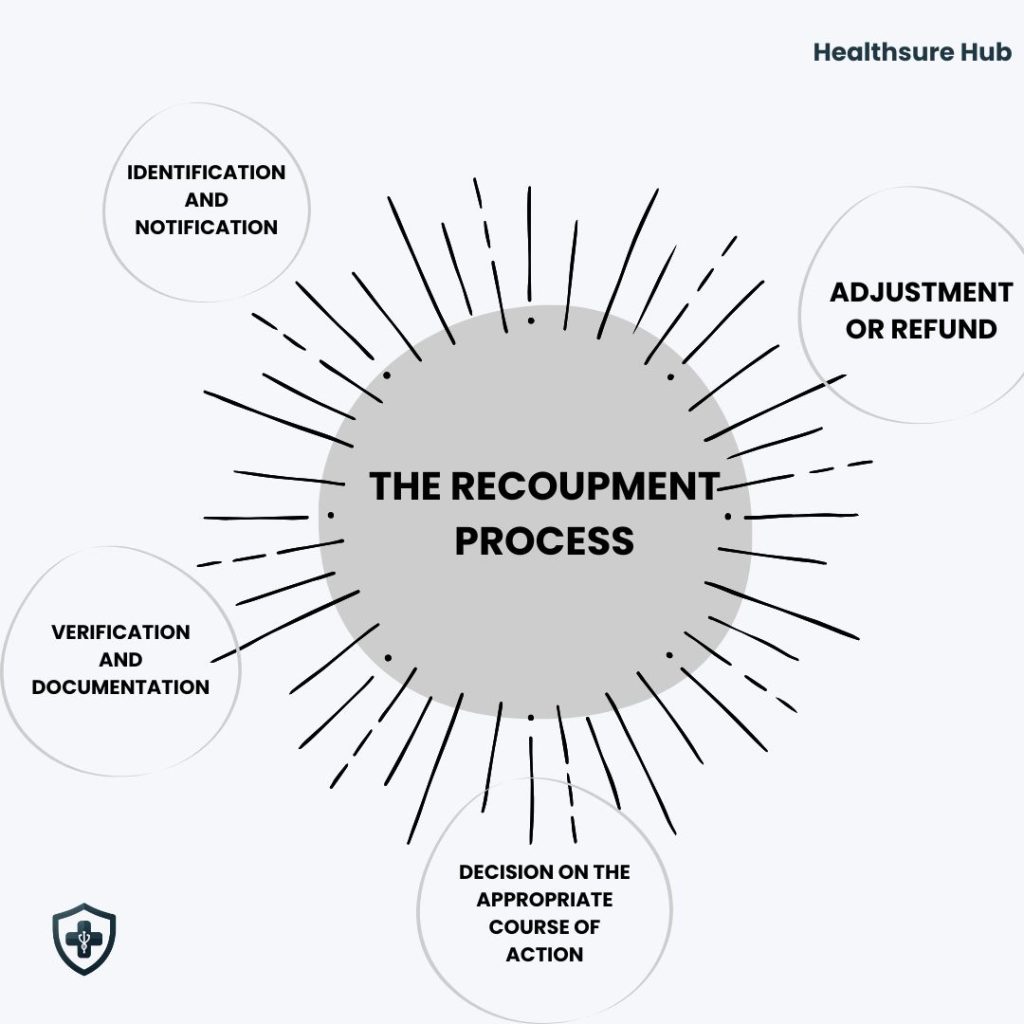
The Recoupment Process
Identification and Notification
Recoupment in medical billing begins the moment a payer identifies an overpayment or payment discrepancy. This detection can occur through multiple channels:
- Routine audits – Insurance companies and government payers like Medicare and Medicaid periodically audit claims to ensure compliance and accurate reimbursement.
- Claims reviews – During processing, automated or manual checks can flag duplicate payments, incorrect codes, or payments that exceed contracted rates.
- Automated detection systems – Many insurers now use AI-driven or rules-based systems to detect anomalies in submitted claims, such as unusually high service volumes or mismatched CPT/HCPCS codes.
Once identified, the payer sends a formal recoupment notice to the provider. This notice typically includes:
- The overpaid amount
- The specific claim(s) involved
- The reason for recoupment (e.g., duplicate claim, incorrect modifier, COB error)
- Deadlines for repayment, response, or dispute
Verification and Documentation
Before taking any action, the provider must carefully verify the recoupment request. This involves:
- Claim review – Compare the claims listed in the notice against your billing system, including dates of service, CPT/HCPCS codes, units, and amounts paid.
- Payment reconciliation – Cross-check the EOBs/ERAs (Explanation of Benefits / Electronic Remittance Advice) with the amounts received. Look for duplicate payments, misapplied funds, or system errors.
- Supporting documentation – Collect medical records, prior authorizations, contracts, and coding notes to support your case. Documentation should clearly demonstrate the medical necessity, correct coding, and eligibility of the claims.
- Contract review – Check your agreements with payers to ensure that any adjustments, bundling rules, or reimbursement caps are properly applied.
This step ensures the recoupment request is valid, or provides the foundation for an appeal if there are discrepancies.
Decision: Repay, Adjust, or Appeal
After verification, the provider must decide the appropriate course of action:
- Repay – If the recoupment request is accurate and supported by documentation, the provider should promptly repay the overpaid amount. Early repayment can reduce interest, penalties, or further scrutiny.
- Adjust future payments – Some payers allow the overpaid amount to be offset against upcoming claims. This method can reduce immediate cash flow strain, particularly for larger recoupments.
- Appeal – If discrepancies or errors are found, such as a misapplied code or mistaken duplicate payment, the provider can file an appeal. An appeal should include:
- A clear explanation of the discrepancy
- Supporting documentation and corrected claims
- References to payer policies or CMS guidelines
Adjustment or Refund
Once the decision is made, providers handle the recoupment in medical billing through financial adjustments:
- Direct refund – Return the overpaid amount to the payer via check, electronic transfer, or the method specified by the insurer.
- Claim adjustment/offset – Apply the recouped amount to future claims or payments, ensuring proper accounting in the practice management system.
Providers should follow payer instructions exactly to avoid additional errors, penalties, or compliance issues.
Impact of Recoupment on Healthcare Providers
Recoupment isn’t just a line item on a statement, it can ripple through a practice in ways that go far beyond dollars and cents. Recoupment in medical billing can put:
- Financial Pressure – When a payer takes back funds, it directly impacts your cash flow. Even a small recoupment can create budget gaps, affecting everything from payroll to supplies. For smaller practices, this can feel like a sudden financial jolt.
- Operational Strain – Resolving a recoupment takes time and attention. Staff must dig through claims, pull records, and compile documentation—all while keeping day-to-day operations running smoothly. These extra hours can slow down new claims and create bottlenecks in the revenue cycle.
- Compliance Concerns – Recurring recoupments can draw the eye of auditors. Even unintentional errors can trigger penalties or heightened scrutiny from payers or regulatory bodies, adding stress to the administrative workload.
- Relationship Challenges – Frequent recoupments can strain relationships with insurers. Delays, disputes, or misunderstandings may make future claims more complicated and require extra effort to maintain smooth communication.
For many providers, especially small practices, recoupment in medical billing isn’t just a financial hiccup. It’s a reminder of why proactive revenue cycle management, accurate billing, and strong documentation practices are so essential. When you’re prepared, you can respond quickly, protect your revenue, and keep your focus on what matters most: patient care.
Conclusion
Recoupment in medical billing is an essential safeguard in medical billing, ensuring accurate payments and compliance with contractual and regulatory standards. While overpayments are sometimes unavoidable, providers can protect their revenue and streamline operations by understanding the causes, managing requests efficiently, and implementing preventive measures.
Whether through staff training, internal audits, updated software, or outsourcing to a skilled medical billing company, proactive management of recoupment is critical for maintaining financial stability and operational efficiency in any healthcare practice.