Medical billing denials are no longer occasional setbacks—they are a persistent threat to healthcare revenue. Even with advanced EHR systems, automated claim scrubbing, and expanded payer connectivity, denial rates continue to rise across both public and commercial insurers. Each denied claim represents more than delayed reimbursement; it signals breakdowns in documentation, coding, eligibility, or workflow that quietly erode financial stability over time.
Understanding the top 10 denials in medical billing is now essential for any organization aiming to protect cash flow and reduce operational waste. We examine the top 10 denials in medical billing, the common denial types, why they occur, and how targeted prevention strategies can transform denials from recurring losses into opportunities for measurable revenue cycle improvement.
What Claim Denials Mean in Medical Billing
Claim denials occur when an insurance payer reviews a processed claim, finds it technically correct, but based on policy determines that the payment will not be issued, either in full or in part. This decision is communicated through an Explanation of Benefits (EOB) or Electronic Remittance Advice (ERA) and is accompanied by standardized denial codes, often referred to as CARC or RARC codes. Among these, the top 10 denials in medical billing represent the most frequent obstacles that practices encounter.
Denials differ from rejections in both timing and cost. A rejected claim fails basic validation checks and is returned before adjudication. A denied claim, however, has already passed through payer processing and therefore requires manual correction, documentation review, or appeal, making it significantly more expensive to resolve.
It’s also important to distinguish denials from payment adjustments like sequestration in medical billing, which reduce Medicare reimbursements due to federal policy rather than eligibility, coding, or documentation errors.
Industry analyses consistently show that more than half of healthcare organizations or 54% to be exact report that denial rates have increased these past years. Across revenue cycle benchmarks, claim denial statistics show that denials cost an average of $25–$117 per claim to rework, excluding the opportunity cost of delayed cash flow.
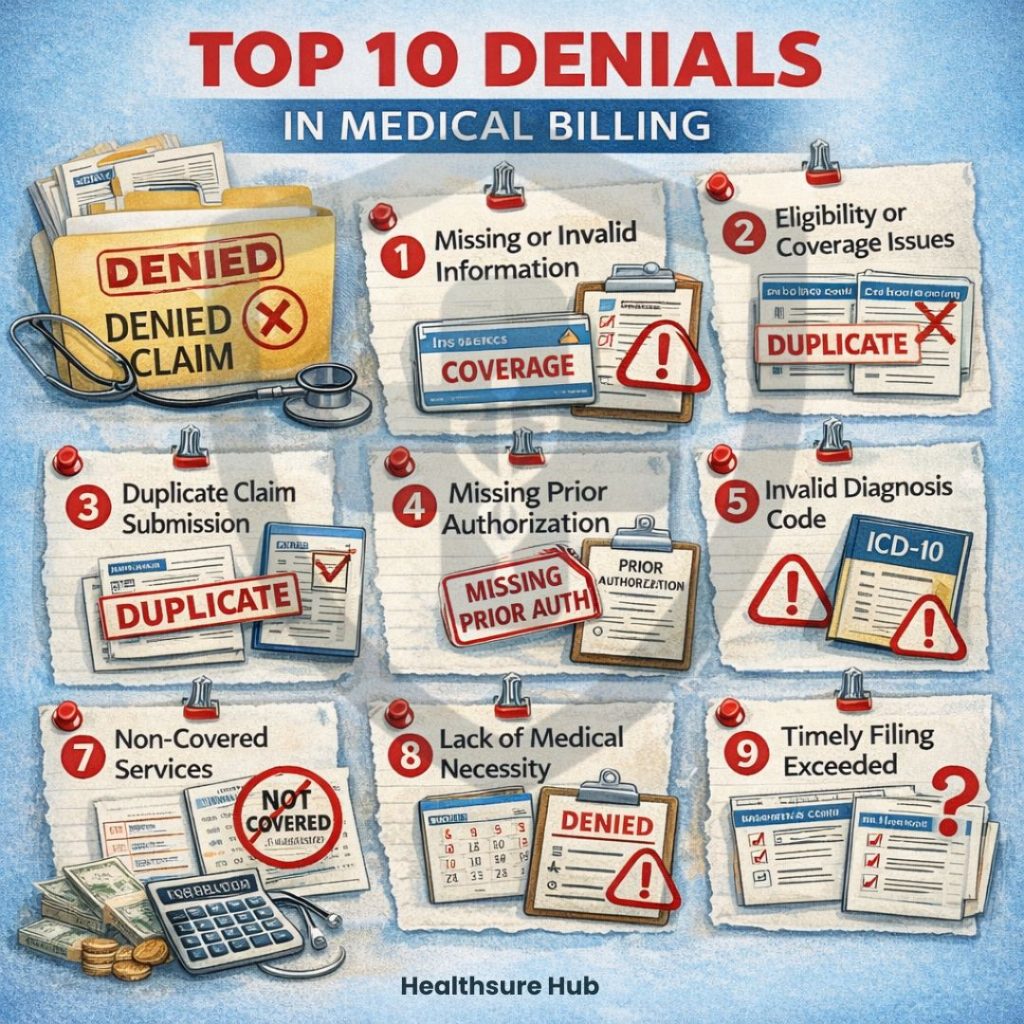
Top 10 Denials in Medical Billing
| Rank | Denial Type | Common Denial Codes | Preventable |
| 1 | Missing or invalid information | CO-16 | Yes |
| 2 | Eligibility or coverage issues | CO-109 | Yes |
| 3 | Duplicate claim submission | CO-18 | Yes |
| 4 | Missing prior authorization | CO-197 | Yes |
| 5 | Invalid diagnosis code | CO-167 | Yes |
| 6 | Invalid procedure code | CO-181 | Yes |
| 7 | Non-covered services | PR-96 | Partially |
| 8 | Lack of medical necessity | CO-50 | Often |
| 9 | Timely filing exceeded | CO-29 | Rarely |
| 10 | Coordination of benefits errors | CO-22 | Yes |
Missing or Incomplete Patient Information (CO-16)
Missing or inaccurate demographic data remains the single most common denial when talking about the top 10 denials in medical billing. Even minor discrepancies, such as a mismatched date of birth or incorrect subscriber ID, can halt claim processing entirely. Primary causes include outdated insurance cards, rushed intake workflows, and inconsistent data verification.
Effective prevention relies on real-time eligibility checks, standardized intake fields, and front-end accountability. When corrected early, CO-16 denials are among the fastest to resolve and most cost-effective to prevent.
Eligibility and Coverage Denials (CO-109)
Eligibility denials occur when a patient’s insurance coverage is inactive or does not apply on the date of service. Coverage lapses, plan changes, and network restrictions frequently trigger this denial category.
Eligibility denials are especially costly because they often require rebilling to secondary insurance or patient responsibility.
Best practices include verifying benefits during scheduling, confirming coverage at check-in, and documenting network participation clearly before services are rendered.
Duplicate Claim Denials (CO-18)
Duplicate claims arise when identical services are submitted multiple times for the same patient, provider, and date of service, or when the systems aren’t synced correctly. This commonly occurs when billing teams resubmit claims prematurely due to unclear claim status. Duplicate denials increase payer scrutiny and can delay legitimate payments. This commonly occurs when billing teams resubmit claims prematurely due to unclear claim status or delayed payment posting in medical billing.
Prevention depends on claim status transparency, ERA review discipline, and defined resubmission timelines within billing systems. Monitoring the top 10 denials in medical billing regularly can reduce duplicate claim submissions significantly.
Missing or Invalid Prior Authorization (CO-197)
One of the top 10 denials in medical billing is because of invalid proper documentation. Certain procedures such as surgeries or imaging require prior authorization. Prior authorization denials occur when required approvals are missing, expired, or mismatched with billed services. High-risk areas include imaging, specialty procedures, and therapies.
Claims denied for missing prior authorization are rarely approved afterward, so verifying authorizations before submitting claims is critical to avoid delays and lost revenue. Strong workflows include authorization tracking within the EHR, payer-specific requirement lists, and pre-service validation checkpoints.
Invalid or Unsupported Diagnosis Codes (CO-167)
One of the top 10 denials in medical billing is because of invalid or unsupported diagnosis codes. These occur when the diagnosis submitted doesn’t clearly support the billed services. Payers require codes that justify medical necessity for each procedure.
Common causes include using overly generic ICD-10 codes, outdated diagnoses, or insufficient documentation. Prevention involves keeping ICD-10 codes updated quarterly, staying informed about payer policies, and fostering closer collaboration between clinical and coding teams to ensure accurate, specific documentation. Awareness of the top 10 denials in medical billing helps coders focus on accuracy.
Invalid or Unsupported Procedure Codes (CO-181)
Procedure code denials occur when CPT or HCPCS codes conflict with payer rules, diagnosis support, or bundling requirements.
These denials often signal fee schedule misalignment or missed National Correct Coding Initiative (NCCI) edits.
Reducing CO-181 denials requires continuous coder education, claim scrubber use, and payer-specific rule validation before submission.Correctly coding the top 10 denials in medical billing reduces repetitive workflow errors.
Non-Covered Services (PR-96)
Non-covered service denials arise when a payer determines that a service falls outside the patient’s benefit plan. Even clinically appropriate services may be excluded based on policy design. These denials shift financial responsibility to patients, increasing billing friction.
Effective mitigation includes benefit verification during scheduling and clear patient communication regarding coverage limitations.
Lack of Medical Necessity (CO-50)
Medical necessity denials occur when documentation fails to demonstrate that a service was deemed as medically necessary. If the payer fails to see an adequate clinical justification, the claim will be denied even if the procedure was needed. These denials are increasing due to automated medical policy enforcement and AI-driven claim reviews.
Strong documentation practices, precise diagnosis coding, and payer policy alignment significantly improve approval rates. Monitoring the top 10 denials in medical billing can reduce these occurrences over time.
Timely Filing Denials (CO-29)
Timely filing denials result from claims submitted after payer-defined deadlines, which range from 90 to 365 days, depending on the payer’s policy. Because late claims are rarely approved, it’s crucial to track submission deadlines carefully. Using automated alerts, payer calendars, and daily claim checks can help ensure claims are filed on time and reduce the risk of CO-29 denials.
Coordination of Benefits Errors (CO-22)
These happen when it’s unclear which payer is responsible for payment, often affecting patients with multiple coverages like employer insurance plus Medicare. COB denials can delay reimbursement for weeks or even months.
Preventing them requires accurately sequencing payers, regularly updating coverage information, and confirming patient insurance details before submitting claims.
Root Causes Behind the Top 10 Denials in Medical Billing
Despite surface-level differences, the top 10 denials in medical billing consistently originate from four upstream failure points:
- Patient access and registration inaccuracies – Even minor errors in patient demographics, insurance ID members, or date of birth can result in an immediate claim denial. Most commonly claims get denied because of misspelled name or missing subscriber or guarantor information. Studies even suggest that up to 35% of denials originate from registration errors.
- Authorization and coverage verification gaps – Missing authorization is one of the top three reasons for denials across multiple specialties. Claims for services requiring prior authorization, referrals, or specific plan coverage often fail if requirements aren’t met.
- Coding and documentation misalignment – Nearly 20% of all claims are denied, mostly because of coding and documentation errors. Incorrect or inconsistent coding is a major driver of denials. Payers rely on accurate CPT, HCPCS, and ICD-10 codes linked to proper documentation.
- Administrative timing and submission breakdowns – Late claims, duplicate submissions, and mismanaged coordination of benefits create denials even when clinical documentation is flawless.
Addressing these areas proactively yields the highest reduction in denial volume and fastest improvement in first-pass acceptance rates.
Why the Top 10 Denials in Medical Billing Matter More in 2025
In 2025, the top 10 denials in medical billing are more important than ever. These denials are a growing threat to healthcare revenue. They are rising because of errors in data, outdated technology, and stricter AI checks by payers. In fact, 41% of providers say that at least one in ten claims they submit gets denied, forcing them to redo and resubmit claims. More precisely, denial trends are evolving due to:
- Increased payer automation and AI audits – Many payers now use AI to automatically flag or deny claims, even for minor errors such as incorrect ICD-10 codes or missing modifiers.
- Rising operational costs – Declining reimbursements combined with higher administrative expenses make unpaid claims a serious threat to the financial health of healthcare practices.
- Stricter medical necessity requirements – Payers are enforcing medical necessity rules more rigorously, making proper documentation and coding essential for claim approval.
- Tighter authorization and eligibility checks – Claims are increasingly denied when prior authorizations or patient eligibility details are incomplete or incorrect.
- Heightened regulatory compliance – Adhering to laws like the No Surprises Act, along with evolving and complex coding standards, has made accurate billing more critical than ever.
Practices that proactively track the top 10 denials in medical billing can improve first-pass claim acceptance rates. Regular staff training on the top 10 denials in medical billing ensures that common errors are identified before submission.
The True Financial Impact of the Top 10 Denials in Medical Billing
Claim denials aren’t just an inconvenience, they directly erode revenue, increase administrative burden, and strain the staff. Understanding the real cost of denials helps organizations prioritize prevention strategies and make informed investments in workflows and technology. The top 10 denials in medical bill affect the:
Direct Financial Costs
On average, each denied claim costs between $25 and $30 to rework in staff time, not including the lost opportunity cost of delayed payment. Even when claims are paid, denial-related delays often result in partial reimbursements or underpayment in medical billing, requiring additional follow-up.
Practices with high denial rates, ranging from 10 to 15 percent, can lose thousands or even tens of thousands of dollars per month, depending on the volume of claims submitted. Reworking these claims involves significant staff time spent researching errors, correcting details, and resubmitting claims, and in many cases, it also requires additional effort to navigate appeals when a claim cannot be resolved immediately.
Extend Accounts Receivable and Disrupt Cash Flow
Denied claims significantly extend accounts receivable (A/R) days, with the average delay for denied claims ranging from 30 to 90 days. This disruption in cash flow can affect every aspect of practice operations, from payroll to supply purchasing, and can be particularly challenging for smaller practices, where a single large denial may create operational bottlenecks. For instance, a medium-sized outpatient clinic processing 2,000 claims per month could face over $60,000 in delayed revenue due to just a 10 percent denial rate. Tracking the top 10 denials in medical billing allows practices to reduce delays in cash flow.
Administrative and Operational Burden
Each denied claim requires staff to manually investigate the issue, correct errors, and resubmit the claim. This diverts time and resources away from patient care and proactive billing initiatives. Over time, repetitive denials contribute to burnout among billing staff and increased turnover, compounding costs associated with hiring and training new employees.
Opportunity Cost
Denials prevent first-pass reimbursement, meaning the practice waits longer to receive payment. High denial rates can also trigger payer audits, which further consume staff time and increase the risk of compliance penalties. Beyond financial implications, denials can confuse patients about their financial responsibility, potentially eroding trust and satisfaction. Practices that maintain denial rates below five percent not only improve their financial outcomes but also enhance the patient experience, supporting better retention and lower readmission risks.
Conclusion
The top 10 denials in medical billing are predictable, measurable, and largely preventable. Most denials originate before the claim is submitted, making front-end accuracy the most powerful lever for revenue protection.
Organizations that align patient access, clinical documentation, coding accuracy, and billing workflows experience faster payments, lower administrative burden, and stronger financial performance while reducing the top 10 denials in medical billing.