Underpayments in medical billing are one of the most overlooked threats to a healthcare organization’s financial health. Imagine delivering a critical service, whether it’s an inpatient procedure, outpatient visit, or therapy session, and receiving only 80% of the payment you’re owed. Over time, these shortfalls can quietly add up to significant revenue losses, affecting operations, staffing, and even patient care.
Understanding what underpayment in medical billing is, why it occurs, and how to identify and prevent it is essential for hospitals, physician practices, and specialty providers aiming to protect their financial performance.
What Is Underpayment in Medical Billing?
Underpayment in medical billing occurs when a healthcare provider receives less reimbursement than what is contractually or legally owed for services rendered. Unlike outright denials, underpayments are often subtle—small amounts on individual claims that accumulate over time, quietly eroding your revenue.
These shortfalls can arise from a variety of factors: payer errors, misapplied contract terms, coding inaccuracies, incomplete documentation, or system and process gaps within the healthcare organization itself. Understanding the root causes is essential, because without addressing them, even the most robust billing operations can leave money on the table.
Why Underpayment in Medical Billing Matter
- Disrupted cash flow can impact daily operations, from paying staff to purchasing medical supplies.
- Financial instability may slow down investments in new technology, infrastructure, or staff training.
- Persistent underpayments can distort financial forecasting and affect strategic decision-making.
Underpayment vs Denial vs Adjustment: Key Differences
One reason underpayments are so costly is that they are often confused with other payment outcomes. Understanding the difference is critical.
| Category | Underpayment | Claim Denial | Contractual Adjustment |
| Payment received | Partial payment | No payment | Reduced per contract |
| Appealable | Yes | Yes | No |
| Visibility | Low | High | Expected |
| Common cause | Payer or billing error | Eligibility, auth, coding | Contracted rates |
| Revenue impact | Ongoing leakage | Delayed cash | Planned reduction |
Denied claims are obvious and usually worked quickly. Underpayment in medical billing, however, can quietly erode revenue over time if payment posting and contract validation processes are weak. In some cases, payers may initially issue full or partial payment and later initiate recoupment in billing, where previously paid funds are taken back due to audits, contract disputes, or documentation issues.
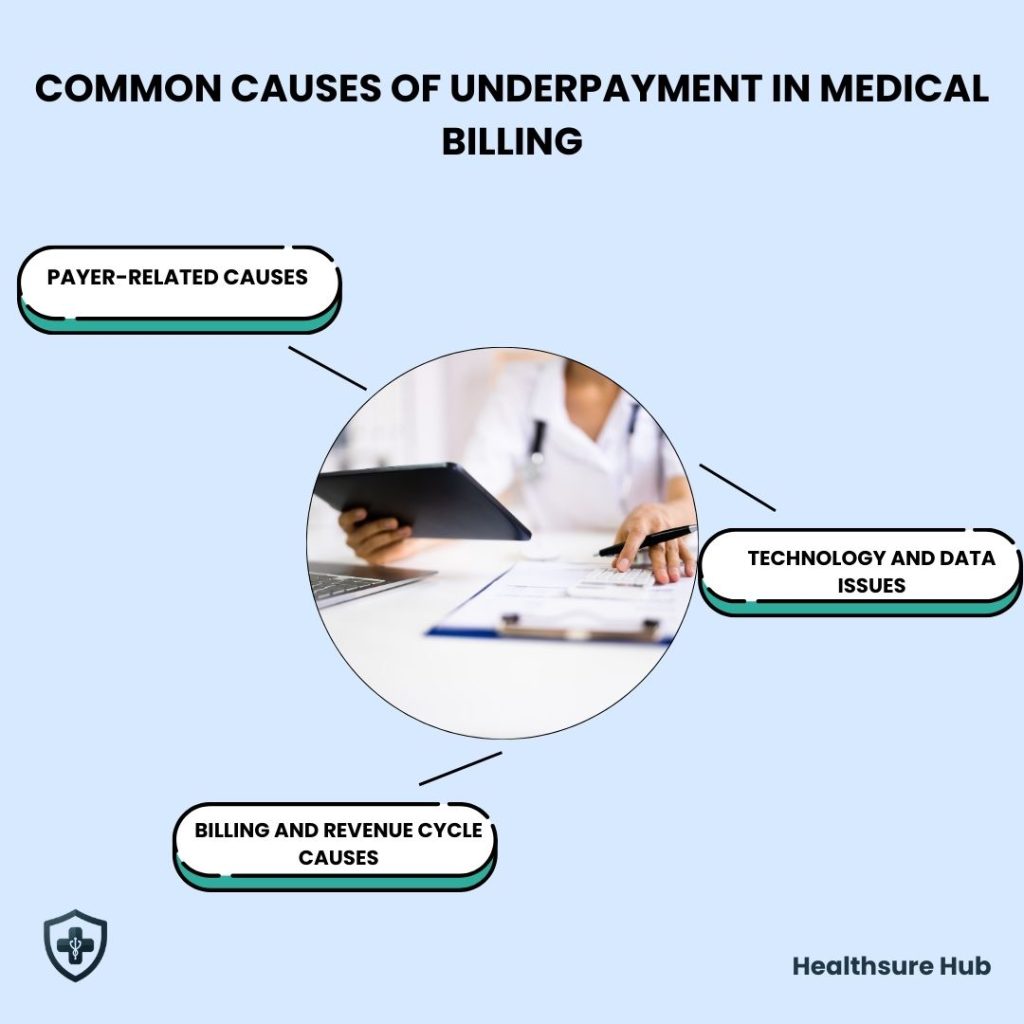
Common Causes of Underpayment in Medical Billing
Underpayments generally fall into three major categories: payer-related issues, revenue cycle issues, and technology or data issues.
Payer-Related Causes of Underpayment in Medical Billing
Many underpayments start on the payer’s side, even when claims are submitted correctly. Insurance contracts are often complex, and small missteps in how they’re applied can lead to lower payments than expected. Certain payers have historically higher denial and underpayment risks. Data shows insurers like UnitedHealthcare and AvMed have denial rates near 33%, which can correlate with increased administrative workload and revenue leakage if not actively managed
For example, payers may misinterpret contract terms such as carve-outs, stop-loss provisions, or “lesser-of” language. When this happens, the reimbursement amount doesn’t reflect what was actually agreed upon. Another common issue is outdated or incorrect fee schedules. If a payer’s system hasn’t been updated with the most recent rates, claims may be priced using old information, resulting in underpayment.
In inpatient settings, DRG downgrades or misassignments can significantly reduce reimbursement. Even a single incorrect DRG can translate into thousands of dollars in lost revenue. Underpayments also occur when payers bundle services that should be reimbursed separately, lowering the total payment for care that was appropriately provided. In addition to underpayments, providers also need to understand mandated payment adjustments such as sequestration in medical billing, which reduces Medicare reimbursements by law rather than payer or coding error.
Finally, processing and system errors can happen on the payer’s end. Even when the contract terms and claim details are accurate, system miscalculations can lead to incorrect allowed amounts and partial payments.
Billing and Revenue Cycle Causes
Underpayment in medical billing isn’t always the payer’s fault. Gaps within a provider’s own billing and revenue cycle processes can also play a major role.
Common issues include medical billing and coding errors, such as incorrect or missing CPT, ICD-10, HCPCS codes, or modifiers, errors that recent statistics on medical billing show account for a significant portion of underpayments. Missing or late charges can also prevent full reimbursement, especially when services are added after a claim is submitted.
Authorization mismatches are another frequent cause. When the authorization on file doesn’t perfectly align with the billed service, payers may reduce payment instead of denying the claim outright.
Underpayments can also stem from payment posting mistakes, where amounts are applied incorrectly, or from misapplied contractual write-offs that reduce balances that should have remained collectible. In some cases, incomplete or insufficient documentation leads payers to reimburse less than expected, even though the service was medically necessary and properly delivered.
The reality is that even small errors, at any point from patient registration to final payment posting, can quietly reduce reimbursement if not caught early on.
Technology and Data Issues
Technology is meant to help identify underpayment in medical billing, but when systems aren’t set up correctly, they can actually make the problem harder to see.
Inaccurate contract loading in billing or contract management systems can cause expected reimbursement calculations to be off from the start. When this happens, underpayments may look “correct” on paper even though they’re not. Many organizations also struggle with noisy payment variance reports that produce too many false positives. This makes it difficult for billing teams to focus on the underpayment in medical billing that truly matter.
A lack of automation can further limit visibility. Without tools that automatically flag payment discrepancies, underpayments often go unnoticed. Finally, poor data integrity makes it hard to trust reimbursement analysis at all. When the data isn’t reliable, identifying real revenue loss becomes a guessing game.
Without strong, dependable systems in place, genuine underpayment in medical billing can easily get lost among irrelevant variances and reporting clutter.
How to Identify Underpaid Claims: A Strategic Approach
Detecting underpaid claims goes far beyond simply checking whether a payment came through. Underpayments are often subtle, small variances per claim that add up to significant revenue loss over time. A proactive, systematic approach is critical to uncovering these hidden gaps and safeguarding your organization’s financial health.
Careful Review of Payer-Provided Documents
Your first line of defense is a careful review of payer-provided documents. Explanation of Benefits (EOB) and Electronic Remittance Advice (ERA) contain detailed breakdowns of how each claim was processed and paid. Comparing the allowed amount against what was actually reimbursed highlights discrepancies quickly.
For effective review consider:
- Focusing on high-dollar claims or frequently performed procedures first, as errors here have the largest impact.
- Tracking recurring underpayments by payers to identify patterns or systemic issues.
- Looking for consistent reductions that don’t match your contract terms.
This step not only identifies underpayment in medical billing but also provides the documentation needed for appeals or discussions with payers.
Leverage Payment Variance Reports Strategically
Payment variance reports are powerful tools for spotting underpayments, but only if they are configured correctly. Poorly designed reports can generate false positives, wasting time and resources.
How to make them work for you:
- Customize reports to focus on material variances that exceed a defined threshold.
- Filter by payer, service type, or CPT/DRG codes to isolate problem areas.
- Integrate historical trends to detect subtle shifts in reimbursement patterns over time.
A well-structured variance report turns raw payment data into actionable insights, helping your team prioritize which claims require investigation first.
Compare Paid Amounts Against Contracted Rates
One of the most reliable ways to catch underpayment for medical billing is by comparing the paid amount with your contracted rates. This requires accurate, up-to-date contract management systems that reflect all negotiated terms.
Best practices:
- Automate the comparison wherever possible to reduce human error.
- Flag claims where the payment deviates from contract terms—even if the variance seems small.
- Investigate unexplained adjustments or write-offs immediately.
By aligning payment data with contract agreements, you can quickly identify both payer errors and internal misapplications that lead to revenue loss.
Watch for Common Red Flags
Certain patterns are almost always indicators of underpayment in medical billing. Being aware of these red flags allows for faster detection and action:
- Consistently low payments – if amounts are regularly just below expectations, this could signal systemic payer miscalculations.
- Payer-specific discrepancies – recurrent underpayments from a single insurer often point to contract misinterpretation or system issues.
- Procedure-specific patterns – specific CPT codes, DRGs, or revenue codes that are repeatedly underpaid may indicate coding disputes or bundling errors.
- Rising contractual write-offs – unexplained increases in write-offs can be a sign that allowed amounts are being incorrectly applied.
Document these patterns carefully, as they provide strong evidence for appeals and help target process improvements.
Implement a Continuous Monitoring Workflow
Identifying underpaid claims isn’t a one-time activity—it’s an ongoing process. Establishing a continuous monitoring workflow ensures issues are caught before they escalate.
Workflow recommendations:
- Schedule weekly or monthly reviews of high-value claims.
- Maintain a tracker for claims under investigation, including payer, service, and variance type.
- Audit a sample of claims quarterly to validate reporting accuracy.
- Share findings with your billing, coding, and managed care teams to address root causes.
How to Recover Underpayment in Medical Billing
Recovering underpayments is less about reactive fixes and more about building a proactive, system-driven strategy. Healthcare organizations that treat underpayments as a critical part of revenue cycle management can safeguard revenue, reduce recurring losses, and strengthen financial stability.
Regular Auditing
The first step is regular auditing. By systematically comparing paid claims against contracts and fee schedules, organizations can spot discrepancies early. These audits reveal patterns in underpayment, highlighting which payers, services, or billing codes consistently fall short. This data-driven insight allows organizations to focus efforts where the financial impact is highest, rather than chasing every minor discrepancy.
Technology and Data Analytics
Technology and data analytics play a pivotal role in this process. Modern billing and contract management systems can automatically flag potential underpayments, validate contract terms, and generate variance reports. When implemented correctly, these tools filter out false positives and spotlight legitimate underpayments, saving time and reducing errors that often occur in manual reviews.
Strategic Payer Engagement
Equally important is strategic payer engagement. Building a consistent, professional line of communication with payer representatives ensures that discrepancies are addressed promptly. Whether it’s clarifying contract terms, correcting misapplied DRGs, or appealing denied claims, proactive communication reduces delays and minimizes the risk of recurring underpayments.
Invest in Staff Expertise
Finally, organizations must invest in staff expertise. Billing and revenue cycle teams should understand not only coding standards and documentation requirements but also the complexities of contracts, payer behavior, and reimbursement trends. Empowering staff to recognize underpayment patterns early allows for immediate corrective action, preventing small errors from escalating into significant revenue losses.

Conclusion
Now that you clearly understand underpayment in medical billing, it’s easy to see why proactive management is essential. Underpayments quietly drain revenue, strain staff, and weaken financial stability if left unchecked.
By combining regular audits, strong payment posting practices, accurate contract management, and proactive payer communication, healthcare organizations can recover lost revenue and prevent future underpayments.