Every year, medical practices lose thousands, sometimes tens of thousands, of dollars due to unnecessary or mismanaged write off in medical billing scenarios. From missed filing deadlines to uncredentialed payers, small operational gaps can quietly erode revenue. Understanding write off in medical billing and how it differs from adjustments is critical for financial stability, regulatory compliance, and the long-term success of any healthcare organization.
Here, we’ll break down what write off in medical billing is, why it happens, how to manage it properly, and the practical steps you can take to minimize revenue loss while maintaining patient trust.
What Is Write Off in Medical Billing?
A write off in medical billing is an amount a healthcare provider chooses not to deduct from a patient’s or insurance balance and does not expect to collect. In simpler terms, it’s money that the practice has “written off” as uncollectible. Write off in medical billing often results from insurance contracts, financial assistance programs, or operational inefficiencies. A write off usually occurs when there is:
- Contractual agreements – Insurance companies often set an “allowed amount” lower than your billed charges.
- Patient inability to pay – Practices sometimes waive balances due to financial hardship.
- Administrative or operational issues – Mistakes in billing, uncredentialed payers, or late claims may require write-offs.
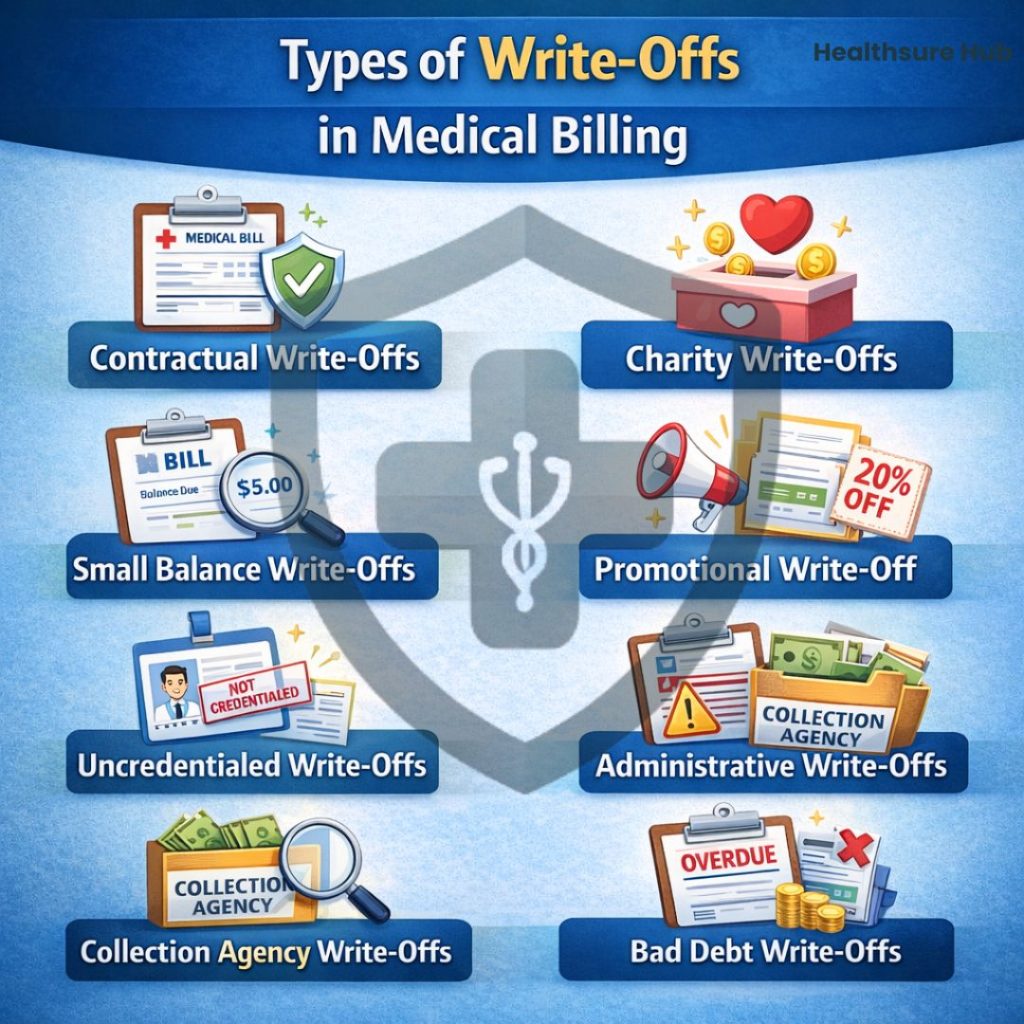
Types of Write-Off in Medical Billing
Write-offs can be categorized into two main groups: necessary/mandatory and inefficiency-driven. Understanding these distinctions is key to maintaining financial control.
Necessary/Mandatory Write-Offs
Contractual Write-Offs
Contractual write off in medical billing is the most commonly used in medical billing. These occur when a healthcare provider accepts a lower, pre-negotiated rate from the insurance company for the services rendered.. For example, if a service is billed at $200 but the insurer allows only $150, the $50 difference is a contractual write-off.
Charity Write-Offs
As the name implies, charity write-off in medical billing are applied when the healthcare provider chooses to forget a portion of the bill for patients usually coming from low-income families. But if you’re a healthcare provider, set a clear line of what falls under charity and what not so that your billing team can account for these types of write-offs without confusion.
Small Balance Write-Offs
As the name suggests, small balance write off in medical billing is provided when the balance is not that high to raise an invoice. Minor amounts (e.g., $5–$20) that are not cost-effective would take a lot of effort, time and money even to pursue them individually. These may be added to a patient’s next visit or written off to avoid administrative overhead.
Promotional Write-Offs
To encourage payment at the time of visit, some practices offer promotional write-offs. Discounts offered to encourage full payment at the time of service, often applied to self-pay patients without insurance coverage.
Unnecessary Write-Offs
Uncredentialed Write-Offs
Uncredentialed write off in medical billing occurs when the provider is not credentialed with a payer, preventing reimbursement even if the patient has active insurance. Proper verification of payer participation can prevent these write-offs. To prevent these types of write-offs, most practices take insurance details and inform patients about their non-coverage and self-pay situations.
Administrative Write-Offs
Situational write-offs approved to resolve patient complaints, disputes, or billing errors. These are discretionary and typically require approval by a provider or practice manager.
Collection Agency Write-Offs
Collection agency write off in medical billing happen when the unpaid balance is transferred to a third-party. As such the amount is no longer pursued by the provider but it’s handled by the collection agency. Hence the name.
Bad Debt Write-Offs
Bed debt write off in medical billing happens when the healthcare provider is no longer interested in pursuing the payment from the patient or the insurance company. This often occurs because of unsuccessful collection efforts, often after several failed attempts.
The Real Impact of Unnecessary Write-Offs
Write off in medical billing is more than just numbers on a ledger, it represents the money your practice could have used to improve operations, invest in staff, or enhance patient care. Even seemingly small amounts can add up quickly if they stem from preventable mistakes.
These unnecessary write-offs also create hidden consequences: distorted financial reports, inaccurate revenue forecasts, and extra administrative work as your team tries to reconcile the losses. Over time, they can slow your practice’s growth, reduce staff morale, and even impact patient experience if resources are stretched thin.
The takeaway? Proper write-off management isn’t just about avoiding lost revenue, it’s about protecting the financial health and operational efficiency of your practice, ensuring every claim is captured accurately and every dollar is accounted for.
How to Write Off Claims Properly
Writing off a claim should never be a rushed or automatic decision. A proper write-off process ensures financial accuracy, compliance with payer rules, and protects your practice from unnecessary revenue loss.
Identify When a Write-Off Is Appropriate
Confirm the balance truly qualifies for a write off in medical billing, such as contractual adjustments, approved hardship cases, or small balances. Common situations include contractual obligations with payers, approved financial hardship cases, small balances that are not cost-effective to pursue, or promotional discounts offered by the practice.
This step is critical because many balances that appear uncollectible at first can still be recovered with correct follow-up or clarification.
Clearly Document the Reason for the Write-Off
Every write-off must have a documented explanation. This creates transparency and protects your practice during audits or financial reviews. Documentation should clearly state whether the write-off resulted from an insurance denial, a contractual allowance, patient financial hardship, or an administrative decision.
Without proper documentation, write-offs can be misclassified, leading to inaccurate reporting and compliance risks.
Follow Established Internal Policies
Written guidelines should define when a write off in medical billing is allowed, who approves it, and any financial limits. This ensures consistency across the billing team and prevents subjective or unauthorized write-offs.
Clear policies also help staff make confident, correct decisions instead of guessing or escalating every case unnecessarily.
Process Write-Offs in a Timely Manner
Once a balance is confirmed as uncollectible, it should be written off promptly. Delays can cause confusion in accounts receivable, distort financial reports, and create extra reconciliation work later.
Timely write-offs keep your billing records accurate and up to date.
Review Write-Offs Regularly
Write-offs should be reviewed on a routine basis, monthly or quarterly, to identify patterns. If certain write-offs occur frequently, such as timely filing denials or uncredentialed claims, they may indicate workflow gaps that need correction.
Regular review turns write-offs into a performance insight, not just a financial loss.
How to Reduce Unnecessary Write-Offs in Medical Billing
Most unnecessary write off in medical billing scenarios are preventable with stronger workflows. Improving a few core workflows can significantly reduce revenue loss and strengthen revenue cycle performance.
- Verify insurance eligibility before services are provided to avoid denials related to inactive coverage or non-covered services. Early verification reduces downstream billing issues and uncollectible balances.
- Improve coding and documentation accuracy through ongoing staff training. Accurate coding minimizes claim rejections, payer disputes, and write-offs caused by billing errors.
- Submit claims promptly and track timely filing limits for each payer. Late claim submission is a common reason for write-offs and directly impacts medical billing collections.
- Establish clear write off in medical billing policies that define when charity care, promotional discounts, and small balance write-offs are permitted. Consistent policies prevent unnecessary write-offs and support accurate financial reporting.
- Monitor write-off trends and denial patterns regularly to identify recurring issues, payer-specific problems, or workflow inefficiencies. Ongoing analysis helps reduce write-offs and improve overall revenue cycle management.
When applied consistently, these strategies help healthcare practices minimize write-offs, improve billing accuracy, and protect revenue.
Best Practices to Minimize Unnecessary Write-Offs
- Verify Insurance – Prevent avoidable write off in medical billing due to inactive coverage
- Improve Coding Accuracy – Train staff on proper documentation and coding to reduce errors and claim denials.
- File Promptly – Submit claims within payer deadlines to avoid timely filing denials.
- Establish Clear Policies – Define when and how charity, promotional, or small balance write-offs are approved to maintain consistency.
- Monitor Trends – Use write off in medical billing data to improve RCM

Impact on Revenue Cycle Management (RCM)
Write-offs affect every phase of the revenue cycle. When they are not tracked, categorized, or controlled correctly, they create financial blind spots that weaken billing performance and cash flow.
Front-End Impact: Eligibility and Patient Intake
Many write-offs begin at the front end. Incomplete insurance verification, inactive coverage, or inaccurate patient responsibility estimates often lead to denied or partially paid claims. While these issues show up later as write-offs, their root cause starts before the claim is even submitted.
Strengthening front-end workflows reduces downstream denials and prevents balances from becoming uncollectible.
Coding and Billing Impact: Claim Accuracy and Denials
During the coding and billing phase, documentation gaps, incorrect modifiers, or mismatched procedure codes commonly trigger payer denials. If these denials are not corrected or appealed within required timeframes, they ultimately turn into write-offs.
What could have been recovered revenue becomes a permanent loss due to preventable billing errors.
Accounts Receivable Impact: Reporting and Cash Flow
Excessive write-offs distort key revenue cycle metrics such as net collection rate, days in A/R, and adjustment ratios. When these figures are inaccurate, leadership cannot reliably assess financial performance or forecast cash flow.
Over time, this leads to poor decision-making and reduced financial visibility.
Compliance and Audit Risk
Inconsistent write-off practices or poor documentation can raise red flags during payer audits. Without clear policies and justification, write-offs may be questioned, increasing the risk of recoupments or compliance issues.
Well-documented, policy-driven write-offs support audit readiness and protect the practice from regulatory exposure.
Long-Term RCM Performance
Unnecessary write-offs directly weaken long-term revenue cycle performance. Revenue lost to avoidable write-offs limits a practice’s ability to invest in staffing, technology, and patient care improvements.
When tracked and analyzed correctly, write-offs become a valuable RCM performance indicator, helping practices identify weaknesses, improve workflows, and strengthen overall financial health.
Conclusion
Write-off in medical billing is unavoidable, but unnecessary write-offs are not. When handled without structure, documentation, or oversight, write-offs quietly drain revenue, distort financial reporting, and weaken the overall revenue cycle. Over time, this erosion affects far more than collections, it impacts staffing, operations, compliance, and patient experience.